National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
National Standards for Culturally and Linguistically
Appropriate Services in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS
Policy and Practice
Office of Minority Health
U.S. Department of Health and Human Services
April 2013

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
i
Table of Contents
Acknowledgments ................................................................................................................. 7
Executive Summary ............................................................................................................... 8
National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care .... 13
The Case for the Enhanced National CLAS Standards ........................................................... 14
Respond to Demographic Changes ..................................................................................................... 15
Eliminate Health Disparities ................................................................................................................ 16
Improve Quality of Services and Care ................................................................................................. 17
Meet Legislative, Regulatory, and Accreditation Mandates .................................................................. 17
Gain a Competitive Edge in the Market Place ...................................................................................... 19
Decrease the Risk of Liability .............................................................................................................. 19
The Enhanced National CLAS Standards .............................................................................. 21
The Standards .................................................................................................................................... 21
Purpose .............................................................................................................................................. 21
Audience ............................................................................................................................................ 21
Components of the Standards ............................................................................................................ 23
Strategies for Implementation ............................................................................................................ 23
Enhancements to the National CLAS Standards ................................................................... 24
Culture ............................................................................................................................................... 24
Health ................................................................................................................................................ 27
Health and Health Care Organizations ................................................................................................ 27
Individuals and Groups ....................................................................................................................... 28
Statement of Intent ............................................................................................................................ 28
Clarity and Action ............................................................................................................................... 29
Standards of Equal Importance .......................................................................................................... 29
Principal Standard and Three Enhanced Themes ................................................................................ 30
New Standard: Organizational Governance and Leadership................................................................. 33

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
ii
Looking Ahead: The Future and the National CLAS Standards.............................................. 34
Continued Enhancements ................................................................................................................... 34
State and Federal Legislation .............................................................................................................. 34
Support and Guidance ........................................................................................................................ 34
Bibliography ........................................................................................................................ 36
The Blueprint ...................................................................................................................... 43
Standard 1: Provide Effective, Equitable, Understandable, and Respectful Quality Care and
Services .............................................................................................................................. 44
Standard 1 ......................................................................................................................................... 44
Purpose .............................................................................................................................................. 44
Components of the Standard .............................................................................................................. 44
Strategies for Achievement of the Principal Standard .......................................................................... 48
Resources .......................................................................................................................................... 48
Bibliography ....................................................................................................................................... 49
Standard 2: Advance and Sustain Governance and Leadership that Promotes CLAS and
Health Equity ...................................................................................................................... 52
Standard 2 ......................................................................................................................................... 52
Purpose .............................................................................................................................................. 52
Components of the Standard .............................................................................................................. 52
Strategies for Implementation ............................................................................................................ 56
Resources .......................................................................................................................................... 57
Bibliography ....................................................................................................................................... 58
Standard 3: Recruit, Promote, and Support a Diverse Governance, Leadership, and Workforce
........................................................................................................................................... 60
Standard 3 ......................................................................................................................................... 60
Purpose .............................................................................................................................................. 60
Components of the Standard .............................................................................................................. 60
Strategies for Implementation ............................................................................................................ 62
Resources .......................................................................................................................................... 63

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
iii
Bibliography ....................................................................................................................................... 64
Standard 4: Educate and Train Governance, Leadership, and Workforce in CLAS ................. 66
Standard 4 ......................................................................................................................................... 66
Purpose .............................................................................................................................................. 66
Components of the Standard .............................................................................................................. 66
Strategies for Implementation ............................................................................................................ 68
Resources .......................................................................................................................................... 69
Bibliography ....................................................................................................................................... 70
Standard 5: Offer Communication and Language Assistance ............................................... 72
Standard 5 ......................................................................................................................................... 72
Purpose .............................................................................................................................................. 72
Components of the Standard .............................................................................................................. 72
Strategies for Implementation ............................................................................................................ 76
Resources .......................................................................................................................................... 76
Bibliography ....................................................................................................................................... 77
Standard 6: Inform Individuals of the Availability of Language Assistance .......................... 79
Standard 6 ......................................................................................................................................... 79
Purpose .............................................................................................................................................. 79
Components of the Standard .............................................................................................................. 79
Strategies for Implementation ............................................................................................................ 81
Resources .......................................................................................................................................... 83
Bibliography ....................................................................................................................................... 83
Standard 7: Ensure the Competence of Individuals Providing Language Assistance ............ 85
Standard 7 ......................................................................................................................................... 85
Purpose .............................................................................................................................................. 85
Components of the Standard .............................................................................................................. 85
Strategies for Implementation ............................................................................................................ 88
Resources .......................................................................................................................................... 89

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
iv
Bibliography ....................................................................................................................................... 90
Standard 8: Provide Easy-to-Understand Materials and Signage ......................................... 93
Standard 8 ......................................................................................................................................... 93
Purpose .............................................................................................................................................. 93
Components of the Standard .............................................................................................................. 93
Strategies for Implementation ............................................................................................................ 95
Resources .......................................................................................................................................... 96
Bibliography ....................................................................................................................................... 97
Standard 9: Infuse CLAS Goals, Policies, and Management Accountability Throughout the
Organization’s Planning and Operations .............................................................................. 99
Standard 9 ......................................................................................................................................... 99
Purpose .............................................................................................................................................. 99
Components of the Standard .............................................................................................................. 99
Strategies for Implementation .......................................................................................................... 100
Resources ........................................................................................................................................ 101
Bibliography ..................................................................................................................................... 102
Standard 10: Conduct Organizational Assessments ........................................................... 103
Standard 10 ..................................................................................................................................... 103
Purpose ............................................................................................................................................ 103
Components of the Standard ............................................................................................................ 103
Strategies for Implementation .......................................................................................................... 105
Resources ........................................................................................................................................ 106
Bibliography ..................................................................................................................................... 107
Standard 11: Collect and Maintain Demographic Data ....................................................... 108
Standard 11 ..................................................................................................................................... 108
Purpose ............................................................................................................................................ 108
Components of the Standard ............................................................................................................ 108
Strategies for Implementation .......................................................................................................... 113

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
v
Resources ........................................................................................................................................ 115
Bibliography ..................................................................................................................................... 116
Standard 12: Conduct Assessments of Community Health Assets and Needs ..................... 118
Standard 12 ..................................................................................................................................... 118
Purpose ............................................................................................................................................ 118
Components of the Standard ............................................................................................................ 118
Strategies for Implementation .......................................................................................................... 120
Resources ........................................................................................................................................ 122
Bibliography ..................................................................................................................................... 122
Standard 13: Partner with the Community ........................................................................ 124
Standard 13 ..................................................................................................................................... 124
Purpose ............................................................................................................................................ 124
Components of the Standard ............................................................................................................ 124
Strategies for Implementation .......................................................................................................... 125
Resources ........................................................................................................................................ 126
Bibliography ..................................................................................................................................... 127
Standard 14: Create Conflict and Grievance Resolution Processes ..................................... 129
Standard 14 ..................................................................................................................................... 129
Purpose ............................................................................................................................................ 129
Components of the Standard ............................................................................................................ 129
Strategies for Implementation .......................................................................................................... 130
Resources ........................................................................................................................................ 131
Bibliography ..................................................................................................................................... 132
Standard 15: Communicate the Organization’s Progress in Implementing and Sustaining
CLAS ................................................................................................................................. 133
Standard 15 ..................................................................................................................................... 133
Purpose ............................................................................................................................................ 133
Components of the Standard ............................................................................................................ 133

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
vi
Strategies for Implementation .......................................................................................................... 134
Resources ........................................................................................................................................ 135
Bibliography ..................................................................................................................................... 136
Appendix A: Glossary ........................................................................................................ 137
Bibliography ..................................................................................................................................... 148
Appendix B: National CLAS Standards Enhancement Initiative .......................................... 155
Background ...................................................................................................................................... 155
Goals ................................................................................................................................................ 155
Development Process ....................................................................................................................... 156
Public Comment ............................................................................................................................... 157
National Project Advisory Committee ................................................................................................ 158
Appendix C: National Project Advisory Committee ............................................................ 162
Appendix D: Crosswalk – National CLAS Standards 2000 and 2012 ................................... 165
Appendix E: Resources ...................................................................................................... 169
List of Figures and Tables
Figure 1: State Legislation...................................................................................................................... 18
Figure 2: Interrelationship of Aspects of Culture..................................................................................... 27
Figure 3: Enhanced National CLAS Standards’ Themes ........................................................................... 31
Figure 4: Phases of the National CLAS Standards Enhancement Initiative ............................................. 156
Figure 5: Advisory Committee Meetings ............................................................................................... 159
Table 1: Blueprint Chapter Structure ...................................................................................................... 43
Table 2: Examples of Promoting CLAS Through Policy and Practice ........................................................ 54
Table 3: Interpreting and Translating ..................................................................................................... 73
Table 4: A Process for Collecting Data .................................................................................................. 114

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Acknowledgments 7
Acknowledgments
This document is the result of a multiyear process that involved many individuals across the country. We
extend our appreciation to them:
o The National Project Advisory Committee (Advisory Committee) members, for their generosity in
sharing their time and expertise and their tireless dedication in the review of numerous drafts of
terminology, documents, and the enhanced National CLAS Standards. A complete list of the
Advisory Committee members appears in Appendix C.
o The individuals and organizations who participated in the public comment period, either by
attending a public comment meeting or by providing online or written submissions. Your input
helped to inform the enhancements to the National CLAS Standards, originally released in 2000.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Executive Summary 8
Executive Summary
Health equity is the attainment of the highest level of health for all people (U.S. Department of Health
and Human Services [HHS] Office of Minority Health [OMH], 2011). Currently, individuals across the
United States from various cultural backgrounds are unable to attain their highest level of health for
several reasons, including the social determinants of health, or those conditions in which individuals are
born, grow, live, work, and age (World Health Organization [WHO], 2012), such as socioeconomic status,
education level, and the availability of health services (HHS Office of Disease Prevention and Health
Promotion [ODPHP], 2010a). Though health inequities are directly related to the existence of historical
and current discrimination and social injustice, one of the most modifiable factors is the lack of culturally
and linguistically appropriate services, broadly defined as care and services that are respectful of and
responsive to the cultural and linguistic needs of all individuals.
Health inequities result in disparities that directly affect the quality of life for all individuals. Health
disparities adversely affect neighborhoods, communities, and the broader society, thus making the issue
not only an individual concern but also a public health concern. In the United States, it has been
estimated that the combined cost of health disparities and subsequent deaths due to inadequate and/or
inequitable care is $1.24 trillion (LaVeist, Gaskin, & Richard, 2009). Culturally and linguistically
appropriate services are increasingly recognized as effective in improving the quality of care and services
(Beach et al., 2004; Goode, Dunne, & Bronheim, 2006). There are numerous ethical and practical reasons
why providing culturally and linguistically appropriate services in health and health care is necessary,
including the following, which have been identified by the National Center for Cultural Competence
(Cohen & Goode, 1999, revised by Goode & Dunne, 2003):
1. To respond to current and projected demographic changes in the United States.
2. To eliminate long-standing disparities in the health status of people of diverse racial, ethnic
and cultural backgrounds.
3. To improve the quality of services and primary care outcomes.
4. To meet legislative, regulatory and accreditation mandates.
5. To gain a competitive edge in the market place.
6. To decrease the likelihood of liability/malpractice claims.
The six reasons for the implementation of cultural competency as described by the National Center for
Cultural Competence fall into two frequently cited overarching philosophies: one that pertains to social
justice and the other that pertains to standards of business. The social justice philosophy emphasizes
diversity and the improvement of services to underserved populations, while the standards of business
philosophy focuses on strengthening business practices and business development.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Executive Summary 9
The enhanced National Standards for Culturally and Linguistically Appropriate Services (CLAS) in Health
and Health Care, known as the enhanced National CLAS Standards, from the Office of Minority Health at
the U.S. Department of Health and Human Services are intended to advance health equity, improve
quality, and help eliminate health care disparities by providing a blueprint for individuals and health and
health care organizations to implement culturally and linguistically appropriate services. The enhanced
National CLAS Standards align with the HHS Action Plan to Reduce Racial and Ethnic Health Disparities
(HHS, 2011) and the National Stakeholder Strategy for Achieving Health Equity (National Partnership for
Action to End Health Disparities, 2011a), which aim to promote health equity through providing clear
plans and strategies to guide collaborative efforts that address racial and ethnic health disparities across
the country. Adoption of these Standards will help advance better health and health care in the United
States.
The enhanced National CLAS Standards are built upon the groundwork laid by the original National CLAS
Standards, developed in 2000 by the HHS Office of Minority Health. The original National CLAS Standards
provided guidance on cultural and linguistic competency, with the ultimate goal of reducing racial and
ethnic health care disparities. Over the past decade, the original National CLAS Standards have served as
catalyst and conduit for efforts to improve the quality of care and achieve health equity (e.g., Diamond,
Wilson-Stronks, & Jacobs, 2010; Joint Commission, 2010; Kairys & Like, 2006).
The HHS Office of Minority Health undertook the National CLAS Standards Enhancement Initiative from
2010 to 2012 to recognize the nation’s increasing diversity, to reflect the tremendous growth in the fields
of cultural and linguistic competency over the past decade, and to ensure relevance with new national
policies and legislation, such as the Affordable Care Act. A decade after the publication of the original
National CLAS Standards, there is still much work to be done. Racial and ethnic disparities in health and
health care remain a significant public health issue, despite advances in health care technology and
delivery, even when factors such as insurance coverage, income, and educational attainment are taken
into account (American College of Physicians, 2010; Griffith, Yonas, Mason, & Havens, 2010). Cultural
and linguistic competency strives to improve the quality of care received and to reduce disparities
experienced by racial and ethnic minorities and other underserved populations (Saha, Beach, & Cooper,
2008). Through the National CLAS Standards Enhancement Initiative, a new benchmark is being
established for culturally and linguistically appropriate services to improve the health of all individuals.
The National CLAS Standards Enhancement Initiative’s development process, described in detail in
Appendix B, was informed by three primary sources: public comment, a National Project Advisory
Committee, and a systematic literature review. These three sources of data informed the scope and
direction of the Enhancement Initiative, and, ultimately, the enhanced National CLAS Standards. For
example, the majority of public comments indicated that while the original National CLAS Standards met
the intended needs as a whole, additional context was needed regarding the Standards’ focus and

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Executive Summary 10
purpose, as well as more clearly defined key terminology. Additional comments suggested that the
organizations targeted for implementing the National CLAS Standards should be expanded and that
additional guidance regarding implementation should be provided.
The data collected from public comment, the National Project Advisory Committee, and the systematic
literature review showed strong support for expanding the key concepts of culture and health, which
serve as the conceptual underpinnings of the National CLAS Standards. Adopting a more comprehensive
conceptualization of health requires, by extension, a more inclusive recognition of the variety of
professionals and organizations providing the related care and services. The enhancements related to this
are as follows:
o
Culture
is defined as the integrated pattern of thoughts, communications, actions, customs,
beliefs, values, and institutions associated, wholly or partially, with racial, ethnic, or linguistic
groups, as well as with religious, spiritual, biological, geographical, or sociological characteristics.
Culture is dynamic in nature, and individuals may identify with multiple cultures over the course
of their lifetimes. This definition is adapted from other widely accepted definitions of culture (i.e.,
Gilbert, Goode, & Dunne, 2007; HHS OMH, 2005) and attempts to reflect the complex nature of
culture, as well as the various ways in which culture has been defined and studied across
multiple disciplines.
o
Health
is understood to encompass many aspects, including physical, mental, social, and
spiritual well-being (HHS Indian Health Services [IHS], n.d.; HHS Office of the Surgeon General
[OSG] & National Action Alliance for Suicide Prevention, 2012; WHO, 1946). The World Health
Organization also notes that health is “not merely the absence of disease or infirmity” (WHO,
1946). Health status occurs along a continuum and therefore can range from poor to excellent.
The advancement of health equity allows individuals to experience better health over the course
of their life spans.
o
Audience
The enhanced National CLAS Standards reference both health and health care
organizations to acknowledge those working not only in health care settings, such as hospitals,
clinics, and community health centers, but also in organizations that provide services such as
behavioral and mental health, public health, emergency services, and community health. Any
organization addressing individual or community health, health care, or well-being can benefit
from the adoption and implementation of the National CLAS Standards.
To further reflect the more inclusive nature of the enhanced National CLAS Standards, the
enhanced Standards use the terminology
individuals and groups
in lieu of
patients
and
consumers
.
Individuals and groups
encompass patients, consumers, clients, recipients, families,

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Executive Summary 11
caregivers, and communities. Therefore, the term
individuals and groups
includes anyone
receiving services from a health or health care organization.
Thus, the enhanced National CLAS Standards incorporate broader definitions of culture and health and
aim to reach a broader audience, in an effort to ensure that every individual has the opportunity to
receive culturally and linguistically appropriate health care and services.
The data collected from public comment, the National Project Advisory Committee, and the systematic
literature review also informed several enhancements to the structure and content of the National CLAS
Standards, as follows (see Appendix D for a comparison between the original and enhanced National
CLAS Standards):
o
Statement of Intent:
The enhanced National CLAS Standards include an introductory
statement:
“The National CLAS Standards are intended to advance health equity, improve quality, and help
eliminate health care disparities by establishing a blueprint for health and health care
organizations to:”
The addition of the statement of intent ties the culturally and linguistically competent policies and
practices posed in the enhanced National CLAS Standards directly to the goals of advancing
health equity, improving quality, and eliminating health care disparities.
o
Clarity and Action:
Each of the National CLAS Standards was revised for greater clarity and
focus. In addition, the wording of each of the 15 Standards now begins with an action word to
emphasize how the desired goal may be achieved.
o
Standards of Equal Importance:
The original National CLAS Standards designated each
Standard as a recommendation, mandate, or guideline. The enhanced National CLAS Standards,
however, promote collective adoption of all Standards to promote optimal health and well-being
of all individuals. Each of the 15 Standards should be viewed as an equally important guideline to
advance health equity, improve quality, and help eliminate health care disparities.
o
Principal Standard and Three Enhanced Themes:
The enhanced Standards have been
reorganized to address feedback obtained from the Enhancement Initiative and to improve their
overall intention, clarity, and practicality. The enhanced National CLAS Standards elevate the
previous Standard 1 to the status of Principal Standard and reframe the three themes. The
names of the three themes have been updated both to clarify intent and to broaden the scope of
their interpretation and application.
•
Principal Standard:
Standard 1 has been made the Principal Standard with the
understanding that it frames the essential goal of all of the Standards, and if the other 14

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Executive Summary 12
Standards are adopted, implemented, and maintained, then the Principal Standard will be
achieved.
•
Theme 1:
Governance, Leadership, and Workforce — Changing the name of Theme 1
from Culturally Competent Care to Governance, Leadership, and Workforce provides
greater clarity on the specific locus of action for each of these Standards and emphasizes
the importance of CLAS implementation as a systemic responsibility, requiring the
endorsement and investment of leadership, and the support and training of all individuals
within an organization.
•
Theme 2:
Communication and Language Assistance — Changing the name of Theme 2
from Language Access Services to Communication and Language Assistance broadens
the understanding and application of appropriate services to include all communication
needs and services, e.g., sign language, braille, oral interpretation, and written
translation.
• Theme 3: Engagement, Continuous Improvement, and Accountability — Changing the
name of Theme 3 from Organizational Supports to Engagement, Continuous
Improvement, and Accountability underscores the importance of establishing individual
responsibility for ensuring that CLAS is supported, while maintaining that effective
delivery of CLAS demands action across organizations.
o
New Standard: Organizational Governance and Leadership:
The enhanced National CLAS
Standards emphasize the importance of CLAS being integrated throughout an organization. This
requires a bottom-up and a top-down approach to advancing and sustaining CLAS. Organizational
governance and leadership are key to ensuring the successful implementation and maintenance
of CLAS. In recognition of this, the enhanced National CLAS Standards include a new Standard
focused on the role of governance and leadership as it relates to CLAS. A complete list of all 15
enhanced National CLAS Standards, including the new Standard, can be found at the end of this
executive summary.
This document, the
National Standards for Culturally and Linguistically Appropriate Services in Health and
Health Care: A Blueprint for Advancing and Sustaining CLAS Policy and Practice
(
The Blueprint)
, offers a
user-friendly format for providing comprehensive — but by no means exhaustive — information on each
Standard.
The Blueprint
is an implementation guide for advancing and sustaining culturally and
linguistically appropriate services within health and health care organizations.
The Blueprint
dedicates one
chapter to each of the 15 Standards. These chapters review the Standard’s purpose, components, and
strategies for implementation. In addition, each chapter provides a list of resources that provide
additional information and guidance on that Standard.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Executive Summary 13
National Standards for Culturally and Linguistically Appropriate
Services in Health and Health Care
The National CLAS Standards are intended to advance health equity, improve quality, and help eliminate
health care disparities by establishing a blueprint for health and health care organizations to:
Principal Standard:
1. Provide effective, equitable, understandable, and respectful quality care and services that are
responsive to diverse cultural health beliefs and practices, preferred languages, health literacy,
and other communication needs.
Governance, Leadership, and Workforce:
2. Advance and sustain organizational governance and leadership that promotes CLAS and health
equity through policy, practices, and allocated resources.
3. Recruit, promote, and support a culturally and linguistically diverse governance, leadership, and
workforce that are responsive to the population in the service area.
4. Educate and train governance, leadership, and workforce in culturally and linguistically
appropriate policies and practices on an ongoing basis.
Communication and Language Assistance:
5. Offer language assistance to individuals who have limited English proficiency and/or other
communication needs, at no cost to them, to facilitate timely access to all health care and
services.
6. Inform all individuals of the availability of language assistance services clearly and in their
preferred language, verbally and in writing.
7. Ensure the competence of individuals providing language assistance, recognizing that the use of
untrained individuals and/or minors as interpreters should be avoided.
8. Provide easy-to-understand print and multimedia materials and signage in the languages
commonly used by the populations in the service area.
Engagement, Continuous Improvement, and Accountability:
9. Establish culturally and linguistically appropriate goals, policies, and management accountability,
and infuse them throughout the organization’s planning and operations.
10. Conduct ongoing assessments of the organization’s CLAS-related activities and integrate CLAS-
related measures into measurement and continuous quality improvement activities.
11. Collect and maintain accurate and reliable demographic data to monitor and evaluate the impact
of CLAS on health equity and outcomes and to inform service delivery.
12. Conduct regular assessments of community health assets and needs and use the results to plan
and implement services that respond to the cultural and linguistic diversity of populations in the
service area.
13. Partner with the community to design, implement, and evaluate policies, practices, and services
to ensure cultural and linguistic appropriateness.
14. Create conflict and grievance resolution processes that are culturally and linguistically appropriate
to identify, prevent, and resolve conflicts or complaints.
15. Communicate the organization’s progress in implementing and sustaining CLAS to all
stakeholders, constituents, and the general public.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
The Case for the Enhanced National CLAS Standards 14
The Case for the Enhanced National CLAS Standards
Of all the forms of inequality, injustice in health care is the most shocking and inhumane.
— Dr. Martin Luther King, Jr.
Health equity is the attainment of the highest level of health for all people (HHS OMH, 2011). Currently,
individuals across the United States from various cultural backgrounds are unable to attain their highest
level of health for several reasons, including the social determinants of health, or those conditions in
which individuals are born, grow, live, work, and age (WHO, 2012), such as socioeconomic status,
education level, and the availability of health services (HHS ODPHP, 2010a). Though health inequities are
directly related to the existence of historical and current discrimination and social injustice, one of the
most changeable factors is the lack of culturally and linguistically appropriate services.
Health inequities result in disparities that directly affect the quality of life for all individuals. Health
disparities adversely affect neighborhoods, communities, and the broader society, thus making the issue
not only an individual concern but also a public health concern. In the United States, it has been
estimated that the combined cost of health disparities and subsequent deaths due to inadequate and/or
inequitable care is $1.24 trillion (LaVeist et al., 2009). Culturally and linguistically appropriate services are
increasingly recognized as effective in improving the quality of care and services (Beach et al., 2004;
Goode et al., 2006). By providing a structure to implement culturally and linguistically appropriate
services, the enhanced National CLAS Standards will improve an organization’s ability to address health
care disparities.
There are numerous ethical and practical reasons why providing culturally and linguistically appropriate
services in health and health care is necessary. The following reasons have been identified by the
National Center for Cultural Competence (Cohen & Goode, 1999, revised by Goode & Dunne, 2003):
1. To respond to current and projected demographic changes in the United States.
2. To eliminate long-standing disparities in the health status of people of diverse racial, ethnic
and cultural backgrounds.
3. To improve the quality of services and primary care outcomes.
4. To meet legislative, regulatory and accreditation mandates.
5. To gain a competitive edge in the market place.
6. To decrease the likelihood of liability/malpractice claims.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
The Case for the Enhanced National CLAS Standards 15
The motivations for implementing CLAS are as varied as the approaches different stakeholders are taking
toward implementation, and depend upon the stakeholder’s mission, goals, and sphere of influence
(Betancourt, Green, Carrillo, & Park, 2005). The six reasons for the implementation of cultural
competency as described by the National Center for Cultural Competence fall into two frequently cited
overarching philosophies: one that pertains to social justice (e.g., Kumagai & Lypson, 2009; Sue, 2001)
and the other that pertains to standards of business (Brach & Fraser, 2002). Specifically, reasons number
one and number two are consistent with the social justice philosophy, which emphasizes diversity and the
improvement of services to underserved populations. The remaining reasons are consistent with the
standards of business philosophy, which focuses on strengthening business practices and business
development.
The enhanced National CLAS Standards align with the HHS Action Plan to Reduce Racial and Ethnic
Health Disparities (HHS, 2011) and the National Stakeholder Strategy for Achieving Health Equity
(National Partnership for Action to End Health Disparities, 2011a), which aim to promote health equity
through providing clear plans and strategies to guide collaborative efforts that address racial and ethnic
health disparities across the country. Similar to these initiatives, the enhanced National CLAS Standards
are intended to advance health equity, improve quality, and help eliminate health care disparities by
providing a blueprint for individuals and health and health care organizations to implement culturally and
linguistically appropriate services. Adoption of these Standards will help advance better health and health
care in the United States.
The following sections expound upon the reasons why culturally and linguistically appropriate services in
health and health care are necessary, as listed by the National Center for Cultural Competence.
Respond to Demographic Changes
It is projected that by 2050 the U.S. demographic makeup will be 47% non-Hispanic White, 29%
Hispanic, 13% Black and 9% Asian (Passel & Cohn, 2008). According to the most recent data,
approximately 20% of the U.S. population, or a little over 58 million people, speak a language other than
English at home, and of that 20%, almost 9% (over 24 million people) have limited proficiency in English
(Au, Taylor, & Gold, 2009; U.S. Census Bureau, 2010), which has implications for their proficiency in
health and health care (The Joint Commission, 2010). Given the increasing cultural diversity over the last
several decades (e.g., Genao, Bussey-Jones, Brady, Branch, & Corbie-Smith, 2003; Goode et al., 2006)
and the rapidly changing landscape of health and health care in the United States (Chin, 2000), there is
an increased need for health and health care professionals and organizations to provide effective, high-
quality care that is responsive to the diverse cultural and linguistic needs of individuals served.
The need for culturally and linguistically appropriate care is particularly great since similar demographic
changes have not occurred in the health and health care workforce (e.g., Genao et al., 2003; Institute of
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
The Case for the Enhanced National CLAS Standards 16
Medicine [IOM], 2004; Sullivan & Mittman, 2010). Given the important role that culture plays in health
and health behaviors (Kleinman, Eisenberg, & Good, 1978; Tseng & Streltzer, 2008), the lack of
workforce diversity is significant since it widens the cultural gap that already exists between health and
health care professionals and consumers, which subsequently contributes to the persistence of health
disparities (Brach & Fraser, 2000; Genao et al., 2003). The provision of culturally and linguistically
appropriate services can help to bridge this gap.
Eliminate Health Disparities
The prevalence of health disparities has been well-documented. For example, racial and ethnic minorities
have disproportionately higher rates of chronic disease and disability, higher mortality rates, and lower
quality of care, compared to non-Hispanic whites (e.g., Health Research & Educational Trust [HRET],
2011; IOM, 2003). In addition, even with expanded insurance coverage, racial minorities are less likely to
receive needed behavioral health services comparable to non-Latino Whites (Alegria, Lin, Chen, Duan,
Cook, & Meng, 2012). Health disparities exist beyond racial and ethnic groups; for example, individuals
with lower incomes are more likely to experience preventable hospitalizations compared to individuals
with higher incomes (HHS Centers for Disease Control and Prevention [CDC], 2011). In addition, lesbian
women are less likely to receive preventative cancer screenings than their heterosexual counterparts
(Buchmueller & Carpenter, 2010), and men who have sex with men are less likely to have access to
health and behavioral health care than the general population of men (e.g., Alvy, McKirnan, DuBois,
Ritchie, Fingerhut, & Jones, 2011; Buchmueller & Carpenter, 2010; McKirnan, DuBois, Alvy, & Jones,
2012).
The provision of culturally and linguistically appropriate services is increasingly recognized as a key
strategy to eliminating disparities in health and health care (e.g., Betancourt, 2004; 2006; Brach &
Fraser, 2000; HRET, 2011). Among several other factors, lack of cultural competence and sensitivity
among health and health care professionals has been associated with the perpetuation of health
disparities (e.g., Geiger, 2001; Johnson, Saha, Arbelaez, Beach, & Cooper, 2004). This is often the result
of miscommunication and incongruence between the patient or consumer’s cultural and linguistic needs
and the services the health or health care professional is providing (Zambrana, Molnar, Munoz, & Lopez,
2004). The provision of culturally and linguistically appropriate services can help address these issues by
providing health and health care professionals with the knowledge and skills to manage the provider-
level, individual-level, and system-level factors referenced in the Institute of Medicine’s seminal report
Unequal Treatment
that intersect to perpetuate health disparities (IOM, 2003).
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
The Case for the Enhanced National CLAS Standards 17
Improve Quality of Services and Care
Health and health care professionals and organizations strive to provide high quality services that meet
the needs of all the individuals they serve. High quality care and services are those provided respectfully
and equitably to all populations served (American Medical Association [AMA], 2006; IOM, 2001). A
commitment to high quality services and care is often reflected in organizations’ mission statements or
core values.
Culture influences health beliefs and practices, as well as health seeking behavior and attitudes (IOM,
2003). When health and health care professionals are aware of culture’s influence on health beliefs and
practices, they can use this awareness to consider and address issues such as access to care. This is just
one example of how culturally and linguistically appropriate services can help improve health and health
care quality (Betancourt, 2006). Culturally and linguistically appropriate services are increasingly
recognized as effective in improving the quality of services (Beach et al., 2004; Goode et al., 2006),
increasing patient safety (e.g., through preventing miscommunication, facilitating accurate assessment
and diagnosis), enhancing effectiveness, and underscoring patient-centeredness (e.g., Betancourt, 2006;
Brach & Fraser, 2000; Thom, Hall, & Pawlson, 2004).
Meet Legislative, Regulatory, and Accreditation Mandates
Culturally and linguistically appropriate services are increasingly included in or referenced by local and
national legislative, regulatory, and accreditation mandates. For example, the Patient Protection and
Affordable Care Act (the Affordable Care Act), Pub. L. No. 111-148 (2010), as amended by the Health
Care and Education Reconciliation Act of 2012, Pub. L. No. 111-152 (2012), referred to collectively as the
Affordable Care Act, contains several provisions related to culturally and linguistically appropriate
services. Section 1311(i)(3)(E) of the Affordable Care Act requires that outreach and education efforts by
Navigators – entities that receive grants from health insurance exchanges created under the Affordable
Care Act to assist individuals in accessing and taking advantage of the exchanges – be culturally and
linguistically appropriate. Furthermore, under sections 2715 and 2719 of the Public Health Service Act as
amended by the Affordable Care Act, insurance companies are required to provide certain disclosures and
notices in a culturally and linguistically appropriate manner.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
The Case for the Enhanced National CLAS Standards 18
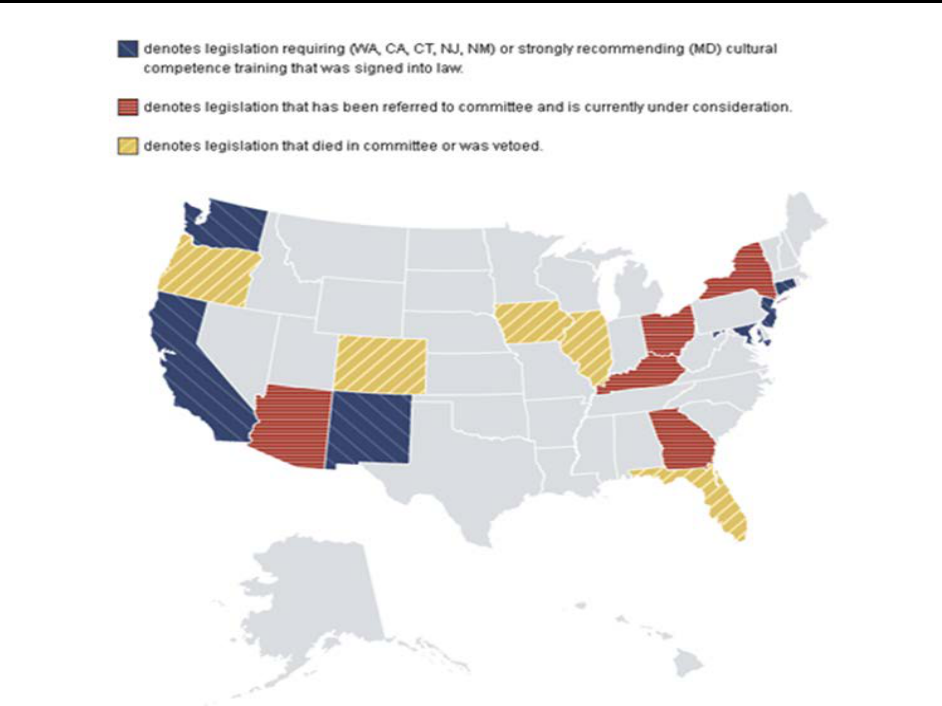
Figure 1: State Legislation
In addition, under Title VI of the Civil Rights Act of 1964, as implemented by Executive Order 13166,
organizations receiving federal funds must take reasonable steps to provide meaningful access to their
programs for individuals with limited English proficiency (Executive Order no. 13,166, 2000).
Furthermore, several states have recognized the importance of cultural and linguistic competency by
legislating cultural and linguistic competency training in health care. These mandates help state health
agencies incorporate cultural and linguistic competency into the health services they provide. As of 2012,
six states have moved to mandate some form of cultural and linguistic competency for either all or a
component of its health care workforce (see Figure 1) (HHS OMH Think Cultural Health, 2012).
Accrediting bodies such as The Joint Commission and the National Committee for Quality Assurance have
established accreditation standards that target the improvement of communication, cultural competency,
patient-centered care, and the provision of language assistance services (Briefer French, Schiff, Han, &
Weinick, 2008; Wilson-Stronks & Galvez, 2007).

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
The Case for the Enhanced National CLAS Standards 19
Gain a Competitive Edge in the Market Place
Culturally and linguistically appropriate services can also help health and health care professionals and
organizations gain a competitive edge in the market place. Although the implementation of culturally and
linguistically appropriate services certainly requires resources, there are numerous business-related
advantages to investing these resources. By implementing culturally and linguistically appropriate services
– including the provision of communication and language assistance, as well as partnerships with the
community – an organization can develop a positive reputation in the service area and therefore expand
its market share. The provision of effective, equitable, understandable, and respectful quality care and
services helps cultivate a loyal consumer base, which then solidifies this market share (AMA, 2006).
As the American Medical Association notes, “a loyal consumer base helps organizations avoid costly
problems, such as high turnover, low utilization rates, and unused capacity” (AMA, 2006, p. 112). In
addition, culturally and linguistically appropriate services, such as assessments of community health
assets and needs, help organizations tailor their services, making the services more cost-effective (e.g.,
Hornberger, Itakura, & Wilson, 1997).
Overall, culturally and linguistically competent practices can help organizations gain a competitive edge in
the market place, as illustrated in the following examples (Alliance of Community Health Plans
Foundation, 2007):
o Holy Cross Hospital in Maryland increased its market share among individuals with limited
English proficiency by creating 68 individual maternity suites with a substantial cultural
competency component in their design. Deliveries at the maternity suites increased from
7,300 to 9,300 annually.
o Contra Costa Health Services in California implemented a Remote Video/Voice Medical
Interpretation Project, which increased the overall effectiveness of interpretation services.
With the addition of this service, the hospital serves twice the number of patients it did
before the service was available, and for significantly lower costs.
Decrease the Risk of Liability
The literature illustrates the vital role communication plays in avoiding cases of malpractice due to
diagnostic and treatment errors (Goode et al., 2006). When communicating with culturally and
linguistically diverse populations, the opportunity for miscommunication and misunderstanding increases,
which subsequently increases the likelihood of errors (Youdelman & Perkins, 2005). These errors, in turn,
can cost millions of dollars in liability or malpractice claims. Culturally and linguistically appropriate
services can reduce the possibility of such errors. For example, a first responder in Florida misinterpreted

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
The Case for the Enhanced National CLAS Standards 20
a single Spanish word, “intoxicado,” to mean "intoxicated" rather than its intended meaning of "feeling
sick to the stomach." This led to a delay in diagnosis, which resulted in a potentially preventable case of
quadriplegia, and ultimately, a $71 million malpractice settlement (Flores, 2006).
The HHS Health Resources and Services Administration [HRSA] found that health professionals who lack
cultural and linguistic competency can be found liable under tort principles in several areas (2005). For
instance, providers may be presumed negligent if an individual is unable to follow guidelines because
they conflict with his/her beliefs and the provider neglected to identify and try to accommodate the
beliefs (HRSA, 2005). Additionally, if a provider proceeds with treatment or an intervention based on
miscommunication due to poor quality language assistance, he/she and his/her organization may face
increased civil liability exposure (DeCola, 2010). Thus, culturally and linguistically appropriate
communication is essential to minimize the likelihood of liability and malpractice claims.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
The Enhanced National CLAS Standards 21
The Enhanced National CLAS Standards
The Standards
The enhanced National Standards for Culturally and Linguistically Appropriate Services in Health and
Health Care from the Office of Minority Health at the U.S. Department of Health and Human Services are
composed of 15 Standards that provide individuals and organizations with a blueprint for successfully
implementing and maintaining culturally and linguistically appropriate services. Culturally and linguistically
appropriate health care and services, broadly defined as care and services that are respectful of and
responsive to the cultural and linguistic needs of all individuals, are increasingly seen as essential to
reducing disparities and improving health care quality.
All 15 Standards are necessary to advance health equity, improve quality, and help eliminate health care
disparities. As important as each individual Standard is, the exclusion of any Standard diminishes health
professionals’ and organizations’ ability to meet an individual’s health and health care needs in a culturally
and linguistically appropriate manner. Thus, it is strongly recommended that each of the 15 Standards be
implemented by health and health care organizations.
Purpose
The purpose of the enhanced National CLAS Standards is to provide a blueprint for health and health care
organizations to implement culturally and linguistically appropriate services that will advance health
equity, improve quality, and help eliminate health care disparities.
Audience
All members of the health and health care community can benefit from the framework offered by the
enhanced National CLAS Standards. The enhanced National CLAS Standards are directed toward a
broader audience than the original Standards in order to address more fully every point of contact
throughout the health care and health services continuum. A wide spectrum of professionals and
organizations influence health and health care every day. The following is a partial list of audiences of the
enhanced National CLAS Standards and how each type of audience might utilize them:
o
Accreditation and Credentialing Agencies:
to assess and compare health care facilities,
health and human service organizations, and providers who offer culturally and linguistically
appropriate services and ensure quality for diverse populations. Institutions such as The Joint
Commission and the National Committee for Quality Assurance have made great strides in
implementing policies and standards to help ensure these quality services.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
The Enhanced National CLAS Standards 22
o
Community-Based Organizations:
to promote quality health care for diverse populations and
to assess and monitor care and services being delivered. The potential advocate audience is
broad and includes: legal services, consumer education agencies, faith-based organizations, and
other local, regional, or national nonprofit organizations that address health and health care
issues.
o
Educators:
to incorporate cultural and linguistic competency into their curricula and to raise
awareness about the impact of culture and language on health and health care services. This
audience would include educators from academic institutions, state health professional licensing
agencies, and educators from legal and social service professions.
o
Governance and Leadership:
to draft consistent and comprehensive laws, regulations, and
contract language. This audience would include federal, state, tribal, and local governments. The
audience would also include the individuals within organizations who are responsible for
developing regulations and contracts, as well as the leadership responsible for decision making
regarding regulations and contracts.
o
Health Care and Service Providers:
to incorporate cultural and linguistic competency into the
delivery of quality health care and services. This audience would include clinicians, practitioners,
and service delivery organizations across health and allied health disciplines, including behavioral
health.
o
Health and Health Care Staff and Administrators:
to implement culturally and linguistically
appropriate services throughout an organization, at every point of contact. This audience would
include employees, contractors, and volunteers serving throughout the organization.
o
Patients/Consumers:
to understand their right to receive accessible and appropriate health
and health care services and to evaluate whether providers can offer them.
o
Public Health Workforce:
to implement cultural and linguistic competency into the provision of
public health services. This audience would include those involved in the behavioral health,
emergency medical services, environmental health, epidemiology, and global health.
o
Purchasers:
to promote the needs of diverse consumers of health benefits, and leverage
responses from insurers and health plans. This audience would include government and employer
purchasers of health benefits.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
The Enhanced National CLAS Standards 23
Components of the Standards
The enhanced National CLAS Standards are built upon the groundwork laid by the original Standards
developed in 2000. The enhanced Standards incorporate broader definitions of culture and health and
aim to reach a broader audience, in an effort to ensure that every individual has the opportunity to
receive culturally and linguistically appropriate health care and services.
The enhanced National CLAS Standards are organized into one Principal Standard and three themes: (1)
Governance, Leadership, and Workforce; (2) Communication and Language Assistance; and (3)
Engagement, Continuous Quality Improvement, and Accountability. Individuals and organizations may
identify or utilize additional standards that are relevant to their mission and services and are encouraged
to add to the National CLAS Standards.
Strategies for Implementation
Implementation of the National CLAS Standards will vary from organization to organization. Therefore,
organizations should identify the best implementation methods appropriate to their size, mission, scope,
and type of services offered. It is also important to develop measures to examine the effectiveness of the
programs being implemented, identify areas for improvement, and identify next steps. Many of these
measures and evaluation strategies may already be in place throughout an organization for the purposes
of accreditation and grant management. Health and human service providers, emergency responders,
community-based organizations, and health care delivery sites (e.g., hospitals, clinics, and community
health centers) will have different goals and expectations for the National CLAS Standards. Therefore,
their strategies for implementation may differ widely.
The enhanced National CLAS Standards and
The Blueprint
include specific implementation strategies to
further the establishment or expansion of culturally and linguistically appropriate services. Prior to
implementation, it is important to have a vision of what culturally and linguistically appropriate services
would look like within the organization and to identify available and required resources (e.g., structure,
funding, and personnel) to ensure success.
Responsibilities associated with implementing the enhanced National CLAS Standards should be
distributed throughout the organization to ensure comprehensive engagement and effectiveness so that
no single individual or department bears the responsibility for the entire organization. For example, some
organizations find it helpful to establish an interdisciplinary or cross-departmental committee that will
help identify, implement, and sustain the elements of a well-developed CLAS plan.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Enhancements to the National CLAS Standards 24
Enhancements to the National CLAS Standards
Data collected during the HHS Office of Minority Health’s National Standards for Culturally and
Linguistically Appropriate Services in Health and Health Care Enhancement Initiative supported the notion
that it was time for an enhancement of the original National CLAS Standards. In the beginning stages of
the Enhancement Initiative, a majority of individuals who provided public comment on the original
National CLAS Standards indicated that though the Standards met their needs as a whole, additional
guidance or direction was needed.
More specifically, individuals and organizations who provided public comment sought clarification on the
Standards’ intention, terminology, and implementation strategies. There was also strong support, from
public comment, the Advisory Committee, and a literature review, for expanding the concepts of health
and culture. The enhanced National CLAS Standards and
The Blueprint
aim to address these issues. The
format of
The Blueprint
reflects the suggestions provided during the public comment period.
The past decade has shown that the National CLAS Standards are dynamic in nature. Therefore, as best
and promising practices develop in the field of cultural and linguistic competency, there will be future
enhancements of the National CLAS Standards. In addition, the Web version of
The Blueprint
will be
updated periodically with additional information and resources as the Standards are disseminated in the
field and as new information is gathered regarding promising implementation and management
strategies.
The following sections discuss the enhancements made to the National CLAS Standards.
Culture
The enhanced National CLAS Standards have adopted an expanded, broader definition of culture.
Specifically, in the enhanced National CLAS Standards, culture refers to “the integrated pattern of
thoughts, communications, actions, customs, beliefs, values, and institutions associated, wholly or
partially, with racial, ethnic, or linguistic groups, as well as with religious, spiritual, biological,
geographical, or sociological characteristics.” This definition is adapted from other widely accepted
definitions of culture (e.g., Gilbert et al., 2007; HHS OMH, 2005) and attempts to reflect the complex and
dynamic nature of culture, as well as the numerous ways in which culture has been defined and studied
across multiple disciplines. Refer to the table below for additional discussion of aspects of culture.
There is considerable recognition that every patient-provider interaction is a cross-cultural interaction and
that the scope of cultural competency in health care should expand to address multiple markers of
difference (Khanna, Cheyney, & Engle, 2009; IOM, 2003). The broader definition of culture adopted in
the enhanced National CLAS Standards mirrors other leading initiatives in the field in terms of scope,
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Enhancements to the National CLAS Standards 25
including Healthy People 2020 from the Department of Health and Human Services (HHS ODPHP, 2010a)
and The Joint Commission (
Advancing Effective Communication, Cultural Competence, and Patient- and
Family-Centered Care: A Roadmap for Hospitals
, 2010). In addition, with the recognition that culture
includes multiple facets and markers of difference, there is an increased opportunity for health
professionals to identify and use similarities to improve health and health care interactions.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Enhancements to the National CLAS Standards 26
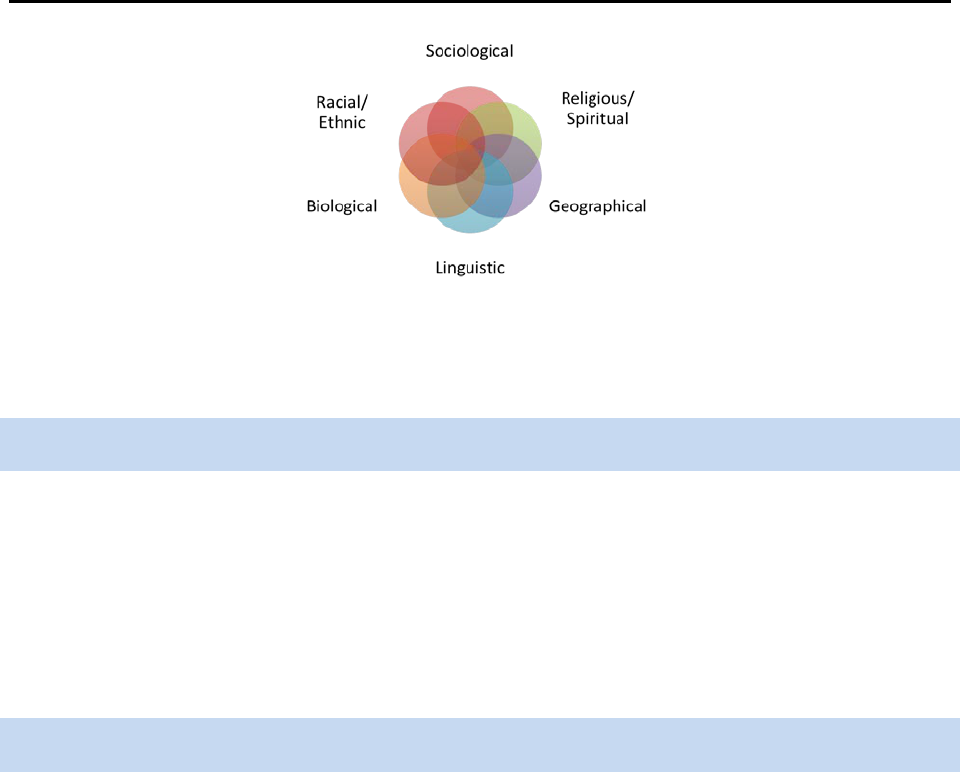
I
ndividuals do not experience their lives or their health through a single lens of identity (e.g., solely race,
gender, or religious); rather, many elements inform their perceptions, beliefs, customs, and reactions
(e.g., Frable, 1997). Figure 2 depicts various aspects of culture through which an individual may
frequently experience his/her cultural identity. For example, an individual’s religious/spiritual
characteristics often overlap with and are informed by the sociological and racial/ethnic groups with
which he/she identifies (e.g., an African American Christian male may experience the world
simultaneously by his race, sex, and religious beliefs). Each of the circles within Figure 2 represents a
very broad area of culture, as described within the definition. These areas are by no means exhaustive,
as there are many other aspects of cultural identity.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Enhancements to the National CLAS Standards 27
(Graves, 2001, revised 2011)
Figure 2: Interrelationship of Aspects of Culture
Health
Health encompasses many aspects, including physical, mental, social, and spiritual well-being (HHS IHS,
n.d.; HHS OSG et al., 2012; WHO, 1946). The World Health Organization also notes that health is “not
merely the absence of disease or infirmity” (WHO, 1946). From this perspective, health status falls along
a continuum and therefore can range from poor to excellent. In addition, how individuals experience
health and define their well-being is greatly informed by their cultural identity. The advancement of
health equity allows the attainment of the highest level of health for all people.
Health and Health Care Organizations
Adopting a more comprehensive conceptualization of health requires, by extension, a more inclusive
recognition of the variety of professionals and organizations providing the related care and services. The
enhanced National CLAS Standards reference both health
and
health care organizations and professionals
to acknowledge those working not only in health care delivery facilities (e.g., hospitals, clinics, community
health centers) but also in organizations that provide services such as behavioral and mental health,
public health, emergency services, and community health and prevention. The National CLAS Standards
are intended for use within all areas of health and human services.
This expansion also acknowledges the growing body of literature that pertains to the social determinants
of health, defined by the World Health Organization as the “the conditions in which people are born,
grow, live, work, and age, including the health system” and the role that social, economic, and
environmental factors, such as socio-economic status and housing, play in health outcomes between
different populations (WHO, 2012). The enhanced National CLAS Standards should be understood as
applicable to hospitals or other health care delivery organizations as well as any public or private
institution addressing individual, family, or community health, health care, or well-being.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Enhancements to the National CLAS Standards 28
Individuals and Groups
To further reflect the more inclusive nature of the enhanced National CLAS Standards, the enhanced
Standards use the terminology
individuals and groups
in lieu of
patients and consumers
.
Individuals and
groups
encompass patients, consumers, clients, recipients, families, caregivers, and communities.
Statement of Intent
In response to public comment and the National Project Advisory Committee feedback requesting further
clarification on the intent of the National CLAS Standards, a statement of intent for the enhanced National
CLAS Standards was crafted and has been added as an introductory statement to the Standards.
The National CLAS Standards are intended to advance health equity, improve quality, and help eliminate
health care disparities by establishing a blueprint for health and health care organizations to:
The addition of the intention statement ties the culturally and linguistically competent policies and
practices posed in the enhanced National CLAS Standards directly to the goals of advancing health equity,
improving quality, and eliminating health care disparities.
Advance Health Equity
Health equity is defined as the attainment of the highest level of health for all people (HHS OMH, 2011).
Currently, many individuals are unable to attain their highest level of health for several reasons, including
social factors such as inequitable access to quality care and individual factors such as limited resources.
Lack of health equity has a significant economic and societal impact. Recent research on the economic
burden of health inequality and health disparities found that:
o Approximately 30.6% of direct medical care expenditures for African Americans, Asians, and
Hispanics were excess costs due to health inequalities (LaVeist et al., 2009).
o Eliminating health inequalities for minorities would have reduced indirect costs associated with
illness and premature death by more than $1 trillion (LaVeist et al., 2009).
Improve Quality
Culturally and linguistically appropriate services and related education initiatives affect several aspects of
an organization’s continuous quality improvement initiatives. For example, research suggests that after
implementation of CLAS initiatives, there are substantial increases in provider knowledge and skill
acquisition and improvements in provider attitudes toward culturally and linguistically diverse patient
populations (Beach et al., 2004). Studies also indicate that patient satisfaction increases when culturally
and linguistically appropriate services are delivered (Beach et al., 2004). At the organizational level,
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Enhancements to the National CLAS Standards 29
hospitals and clinics that support effective communication by addressing CLAS have been shown to have
higher patient-reported quality of care and more trust in the organization (Wynia, Johnson, McCoy,
Passmore Griffin, & Osborn, 2010). Preliminary research has shown a positive impact of CLAS on patient
outcomes (Lie, Lee-Rey, Gomez, Bereknyel, & Braddock, 2010), and a growing body of evidence
illustrates the effectiveness of culturally and linguistically appropriate services in improving the quality of
care and services received by individuals (Beach et al., 2004; Goode et al., 2006).
Help Eliminate Health Care Disparities
Eliminating health care disparities is one of the ultimate goals of advancing health equity. Disparities exist
and persist across many culturally diverse groups, with individuals who identify as racial or ethnic
minorities being less likely to receive preventive health services, even when insured (DeLaet, Shea, &
Carrasquillo, 2002).
The following are a few selected findings featured in the HHS Agency for Healthcare Quality and
Research [AHRQ] 2011 National Healthcare Quality Report and National Healthcare Disparities Report
that highlight the disparities experienced by many in the United States (AHRQ, 2012a, 2012b):
o Access to quality health care remains suboptimal, particularly for minority and low-income
groups.
o Despite improvements in quality, access and disparities have not improved.
o Certain services, geographic areas and populations were found to be in serious need of
improvements in quality and progress in disparities reduction.
As the enhanced National CLAS Standards are disseminated, the inclusion of the statement of intent
within the actual Standards ensures that every person who uses the Standards will understand their
importance. Although this brief introductory statement cannot convey all the potential purpose(s) of the
Standards, it does convey their primary goals.
Clarity and Action
Each of the National CLAS Standards was revised for greater clarity and focus. In addition, the wording of
each of the 15 Standards now begins with an action word to emphasize how the desired goal may be
achieved.
Standards of Equal Importance
The original National CLAS Standards designated each Standard as a recommendation, mandate, or
guideline. The recommendation (original Standard 14) was a suggestion for voluntary adoption by health
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Enhancements to the National CLAS Standards 30
care organizations. The mandates (original Standards 4, 5, 6, and 7) were Federal requirements for all
recipients of Federal funds. The guidelines (original Standards 1, 2, 3, 8, 9, 10, 11, 12, and 13) were
activities recommended for adoption as mandates by Federal, State, and national accrediting agencies.
However, the enhanced National CLAS Standards promote collective adoption of all Standards as the
most effective approach to improve the health and well-being of all individuals. The Standards are
intended to be used together, as mutually reinforcing actions, and each of the 15 Standards should be
understood as an equally important guideline to advance health equity, improve quality, and help
eliminate health care disparities.
Although the enhanced National CLAS Standards do not represent statutory requirements, failure by a
recipient of Federal financial assistance to provide services consistent with Standards 5 through 8 could
result in a violation of Title VI of the Civil Rights Act of 1964 implementing regulation (See 42 USC 2000d
et. Seq. and 45 CFR Part 80). Therefore, although Standards 5 through 8 do not represent legal
requirements in all cases, implementation of these goals will help ensure that health care organizations
and individual providers serve persons of diverse backgrounds in a culturally and linguistically appropriate
manner and in accordance with the law. Advances in technology help health and human service
organizations provide efficient and cost-effective language assistance services (Sperling, 2011). Health
care organizations and individual providers are encouraged to seek technical assistance from the HHS
Office for Civil Rights or review the
HHS Guidance to Federal Financial Assistance Recipients Regarding
Title VI Prohibition Against National Origin Discrimination Affecting Limited English Proficient Persons
document (HHS Office for Civil Rights [OCR], 2003)
to assess whether or to what extent language access
services must be provided in order to comply with the Title VI requirement to take reasonable steps to
provide meaningful access to their programs for persons with limited English proficiency.
Principal Standard and Three Enhanced Themes
The enhanced Standards have been reorganized to address feedback gleaned from the Enhancement
Initiative and to improve their overall intention, clarity, and practicality.
The enhanced National CLAS Standards elevate the previous Standard 1 to the status of a Principal
Standard, add a governance and leadership Standard as Standard 2, and reframe the three themes.
1
1
A crosswalk of the National CLAS Standards 2000 and 2012 may be found in Appendix D.
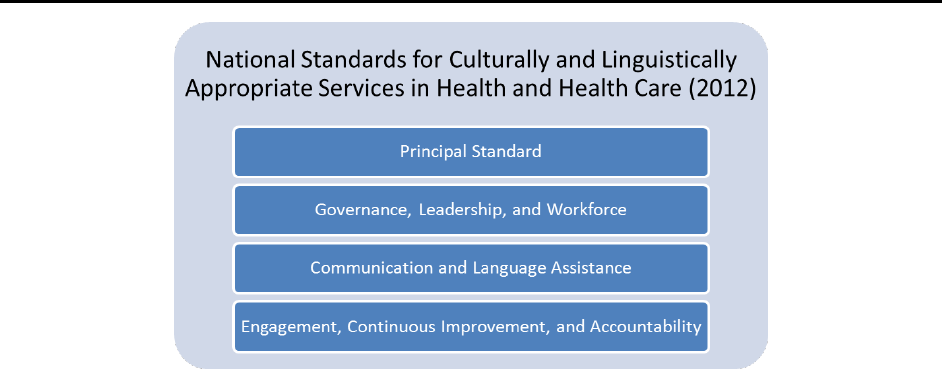
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Enhancements to the National CLAS Standards 31
Figure 3: Enhanced National CLAS Standards’ Themes
The names of the three themes have been updated both to clarify intent and to broaden the scope of
their interpretation and application.
Principal Standard
Standard 1 has been made the Principal Standard with the understanding that it frames the essential goal
of all of the Standards, and if the other 14 Standards are adopted, implemented, and maintained, then
the Principal Standard will be achieved.
1. Provide effective, equitable, understandable, respectful, and quality care and services that are
responsive to diverse cultural health beliefs and practices, preferred languages, health literacy,
and other communication needs.
Theme 1: Governance, Leadership, and Workforce
Changing the name of Theme 1 from
Culturally Competent Care
to
Governance, Leadership, and
Workforce
provides greater clarity on the specific locus of action for each of these Standards and
emphasizes the importance of the implementation of CLAS as a systemic responsibility, requiring the
investment, support, and training of all individuals within an organization.
The Standards in this theme include:
2. Advance and sustain governance and leadership that promotes CLAS and health equity
3. Recruit, promote, and support a diverse governance, leadership, and workforce
4. Educate and train governance, leadership, and workforce in CLAS

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Enhancements to the National CLAS Standards 32
Theme 2: Communication and Language Assistance
Changing the name of Theme 2 from
Language Access Services
to
Communication and Language
Assistance
broadens the understanding and application of appropriate services to include all
communication needs and services, including sign language, braille, oral interpretation, and written
translation.
The Standards in this theme include:
5. Offer communication and language assistance
6. Inform individuals of the availability of language assistance
7. Ensure the competence of individuals providing language assistance
8. Provide easy-to-understand materials and signage
Theme 3: Engagement, Continuous Improvement, and Accountability
Changing the name of Theme 3 from
Organizational Supports
to
Engagement, Continuous Improvement,
and Accountability
underscores the importance of establishing individual responsibility in ensuring that
CLAS is supported, while retaining the understanding that effective delivery of CLAS demands actions
across an organization. This revision focuses on the supports necessary for adoption, implementation,
and maintenance of culturally and linguistically appropriate policies and services regardless of one’s role
within an organization or practice. All individuals are accountable for upholding the values and intent of
the National CLAS Standards.
The Standards in this theme include:
9. Infuse CLAS goals, policies, and management accountability throughout the organization’s
planning and operations
10. Conduct organizational assessments
11. Collect and maintain demographic data
12. Conduct assessments of community health assets and needs
13. Partner with the community
14. Create conflict and grievance resolution processes
15. Communicate the organization’s progress in implementing and sustaining CLAS
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Enhancements to the National CLAS Standards 33
New Standard: Organizational Governance and Leadership
Another theme that emerged from the feedback provided during the Enhancement Initiative was the
importance of CLAS being infused throughout an organization. This requires both a bottom-up
and
a top-
down approach to advancing and sustaining CLAS. Organizational governance and leadership are key to
ensuring the successful adoption, implementation, and maintenance of CLAS. In recognition of this, the
enhanced National CLAS Standards include a new Standard focused on the role of governance and
leadership as it relates to CLAS. This new Standard was placed as the second Standard and within Theme
1, “Governance, Leadership, and Workforce.”
The new second Standard states:
Advance and sustain organizational governance and leadership that promotes CLAS and health equity
through policy, practices, and allocated resources.
The inclusion of a Standard for organizational governance and leadership emphasizes the importance of a
comprehensive effort to infuse culturally and linguistically appropriate services throughout an
organization. The responsibility to embrace CLAS should fall throughout the entire organization. This
comprehensive effort cannot succeed unless the governance and leadership of an organization has
embraced these values and are willing to implement and sustain them. In addition, the scope of
Standards 3 and 4 (Standards 2 and 3 in the original Standards) were expanded to include “governance
and leadership” to continue to emphasize their integral role in the successful adoption of CLAS.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Looking Ahead: The Future and the National CLAS Standards 34
Looking Ahead: The Future and the National CLAS Standards
Since the inception of the original National CLAS Standards in 2000, the fields of cultural and linguistic
competency have proven to be as dynamic as the diversity of our communities and the fields of health
and health care themselves. Looking ahead, the ultimate goal is to ensure that the National CLAS
Standards remain relevant until the next Enhancement Initiative. Following are some of the areas
currently under consideration to achieve this goal.
Continued Enhancements
In recognition of this dynamic landscape, the HHS Office of Minority Health will revisit
The Blueprint
periodically to incorporate new and relevant resources as appropriate. Therefore, a Web version of
The
Blueprint
will be maintained, which will reflect the more comprehensive and up-to-date resource.
In the event that a change in national policy occurs or research is published that impacts the integrity or
validity of any of the Standards or content within the Standard chapters, appropriate revisions will be
made and noted on the Office of Minority Health’s Think Cultural Health website
(www.thinkculturalhealth.hhs.gov).
State and Federal Legislation
State Legislation: Mandating Cultural and Linguistic Competency Training
In the years since the launch of the original National CLAS Standards, a number of states have
implemented legislation pertaining to culturally and linguistically appropriate services (Graves, Like, Kelly,
& Hohensee, 2007; HHS OMH Think Cultural Health, 2012). For many health professionals and
organizations, the original National CLAS Standards served as a driver or model for what the legislation
could include.
Federal Legislation: Affordable Care Act of 2010
The Affordable Care Act of 2010 lays an important foundation for advancing health equity and improving
the quality of services to diverse communities (Andrulis, Siddiqui, Purtle, & Duchon, 2010; Youdelman,
2011). There are numerous provisions in the health care law related to cultural and linguistic
competency, and the enhanced National CLAS Standards serve as a resource, at all levels, in these areas.
Support and Guidance
A recurring theme throughout the public comment portion of the Enhancement Initiative was the request
for additional support and guidance in the implementation and maintenance of the National CLAS
Standards.
The Blueprint
represents the first component of that support and guidance. While
The

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Looking Ahead: The Future and the National CLAS Standards 35
Blueprint
provides strategies for implementation, more targeted discipline- or profession-specific
strategies may be necessary. It is anticipated that as part of the ongoing discussion of these efforts,
collaborations will be formed with the aim of developing discipline specific support and guidance
documents. Additional supporting documents will be made available on the Think Cultural Health website
(www.thinkculturalhealth.hhs.gov).

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Bibliography 36
Bibliography
Alliance of Community Health Plans. (2007).
Making the business case for culturally and linguistically
appropriate services in health care: Case studies from the field
. Retrieved from the Office of
Minority Health website: http://minorityhealth.hhs.gov/Assets/pdf/Checked/CLAS.pdf
Alegria, M., Lin, J., Chen, C., Duan, N., Cook, B., & Meng, X. (2012). The impact of insurance coverage in
diminishing racial and ethnic disparities in behavioral health services.
Health Services Research,
47
(3), 1322-1344. doi:10.1111/j.1475-6773.2012.01403.x
Alvy, L.M., McKirnan, D.J., DuBois, S.N., Ritchie, N., Fingerhut, D., & Jones, K. (2011). Health care
disparities and behavioral health among men who have sex with men.
Journal of Gay and Lesbian
Social Services, 23
, 1-15.
American College of Physicians. (2010).
Racial and ethnic disparities in health care: Updated 2010
.
Retrieved from
http://www.acponline.org/advocacy/where_we_stand/access/racial_disparities.pdf
American Medical Association. (2006).
Improving communication, improving care: How health care
organizations can ensure effective, patient-centered communication with people from diverse
populations
. Retrieved from http://www.ama-assn.org/resources/doc/ethics/pcc-consensus-
report.pdf
Andrulis, D. P., Siddiqui, N. J., Purtle, J., & Duchon, L. (2010).
Patient Protection and Affordable Care Act
of 2010: Advancing health equity for racially and ethnically diverse populations.
Retrieved from
the Joint Center for Political and Economic Studies website:
http://www.jointcenter.org/hpi/sites/all/files/PatientProtection_PREP_0.pdf
Association of American Medical Colleges. (1999).
Contemporary issues in medicine: Communication in
medicine
. Retrieved from
https://members.aamc.org/eweb/DynamicPage.aspx?Action=Add&ObjectKeyFrom=1A83491A-
9853-4C87-86A4-
F7D95601C2E2&WebCode=PubDetailAdd&DoNotSave=yes&ParentObject=CentralizedOrderEntry
&ParentDataObject=Invoice%20Detail&ivd_formkey=69202792-63d7-4ba2-bf4e-
a0da41270555&ivd_prc_prd_key=7A646605-335A-474C-99DD-5F1AD10D96BC
Au, M., Taylor, E., & Gold, M. (2009).
Improving access to language services in health care: A look at
national and state efforts
. Retrieved from
http://www.ahrq.gov/populations/languageservicesbr.pdf
Beach, M. C., Cooper, L. A., Robinson, K. A., Price, E. G., Gary, T. L., Jenckes, M. W., … Powe, N. R.
(2004).
Strategies for improving minority healthcare quality
. (AHRQ Publication No. 04-E008-02).
Retrieved from the Agency of Healthcare Research and Quality website:
http://archive.ahrq.gov/downloads/pub/evidence/pdf/minqual/minqual.pdf

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Bibliography 37
Betancourt, J.R. (2004). Cultural competence – marginal or mainstream movement?
New England Journal
of Medicine, 351
, 953-955.
Betancourt, J.R. (2006).
Improving quality and achieving equity: The role of cultural competence in
reducing racial and ethnic disparities in health care
. (Commonwealth Fund Publication No. 961).
Retrieved from The Commonwealth Fund website:
http://www.commonwealthfund.org/~/media/Files/Publications/Fund%20Report/2006/Oct/Impro
ving%20Quality%20and%20Achieving%20Equity%20%20The%20Role%20of%20Cultural%20Co
mpetence%20in%20Reducing%20Racial%20and%20Ethni/Betancourt_improvingqualityachieving
equity_961%20pdf.pdf
Betancourt, J.R., Green, A.R., Carrillo, J.E., & Park, E.R. (2005). Cultural competence and health care
disparities: Key perspectives and trends.
Health Affairs, 24
, 499-505.
Brach, C., & Fraser, I. (2002). Reducing disparities through culturally competent health care: An analysis
of the business case.
Quality Management in Health Care, 10
, 15-28.
Brach, C., & Fraser, I. (2000). Can cultural competency reduce racial and ethnic health disparities? A
review and conceptual model.
Medical Care Research and Review, 57
, 181-217.
Briefer French, J., Schiff, D., Han, E., & Weinick, R. (2008).
Multicultural health care: A quality
improvement guide
. Retrieved from National Committee for Quality Assurance website:
http://www.ncqa.org/Portals/0/HEDISQM/CLAS/CLAS_toolkit.pdf
Buchmueller T., & Carpenter C.S. (2010). Disparities in health insurance coverage, access, and outcomes
for individuals in same-sex versus different-sex relationships, 2000–2007.
American Journal of
Public Health
.
100
(3), 489-495.
Chin, J.L. (2000). Culturally competent health care.
Public Health Reports, 115
, 25-33.
Cohen, E., & Goode, T.D. (1999), revised by Goode, T.D., & Dunne, C. (2003).
Policy brief 1: Rationale
for cultural competence in primary care
. Washington, DC: National Center for Cultural
Competence, Georgetown University Center for Child and Human Development.
DeCola, A. (2010). Making language access to health care meaningful.
Journal of Law and Health, 58
,
151- 182. Retrieved from
http://www.imiaweb.org/uploads/docs/Making_Language_Access_to_Healthcare_Meaningful.pdf
DeLaet, D. E., Shea, S., & Carrasquillo, O. (2002). Receipt of preventive services among privately insured
minorities in managed care versus fee-for-service insurance plans.
Journal of General Internal
Medicine
,
17,
451–457. doi:10.1046/1525-1497.2002.10512.x
Diamond, L.C., Wilson-Stronks, A., & Jacobs, E.A. (2010). Do hospitals measure up to the National
Culturally and Linguistically Appropriate Services Standards?
Medical Care, 48
, 1080-1087.
Exec. Order No. 13,166, 3 C.F.R. 289 (2000).

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Bibliography 38
Frable, D. E. S. (1997). Gender, racial, ethnic, sexual, and class identities.
Annual Review of Psychology,
48,
139–162. doi:10.1146/annurev.psych.48.1.139
Flores, G. (2006). Language barriers to health care in the United States.
New England Journal of
Medicine
,
355,
229–231. Retrieved from http://www.nejm.org/doi/full/10.1056/NEJMp058316
Geiger, H.J. (2001). Racial stereotyping and medicine: The need for cultural competence.
Canadian
Medical Association Journal, 164
, 1699-1700.
Genao, I., Bussey-Jones, J., Brady, D., Branch, W.T., Corbie-Smith, G. (2003). Building the case for
cultural competence.
American Journal of the Medical Sciences, 326
(3), 136-140.
Goode, T.D., & Dunne, C. (2003).
Policy brief 1: Rationale for cultural competence in primary care
.
Washington, DC: National Center for Cultural Competence, Georgetown University Center for
Child and Human Development.
Gilbert, J., Goode, T. D., & Dunne, C. (2007). Cultural awareness. In
Curricula enhancement module
series.
Retrieved from the National Center for Cultural Competence website:
http://www.nccccurricula.info/awareness/index.html
Goode, T. D., Dunne, M. C., & Bronheim, S. M. (2006).
The evidence base for cultural and linguistic
competency in health care
. (Commonwealth Fund Publication No. 962). Retrieved from The
Commonwealth Fund website:
http://www.commonwealthfund.org/usr_doc/Goode_evidencebasecultlinguisticcomp_962.pdf
Graves, D. (2001).
Your golden rule might not be mine and other lessons learned from cultural
competency.
Workshop presented as part of Year One Orientation at the University of Missouri-
Kansas City School of Medicine.
Graves, D. L., Like, R. C., Kelly, N., & Hohensee, A. (2007). Legislation as intervention: A survey of
cultural competence policy in health care.
Journal of Health Care Law and Policy, 10
(2),
339–361.
Retrieved from http://thecqc.org/uploads/Graves_et_al.pdf
Griffith, D. M., Yonas, M., Mason, M., & Havens, B. (2010). Considering organizational factors in
addressing healthcare disparities: Two case examples.
Health Promotion Practice, 11
(3), 367–
376. doi:10.1177/1524839908330863
Health Research & Educational Trust, Institute for Diversity in Health Management (2011).
Building a
culturally competent organization: The quest for equity in health care.
Retrieved from
http://www.hret.org/quality/projects/resources/cultural-competency.pdf
Hornberger J., Itakura H., & Wilson S.R. (1997). Bridging language and cultural barriers between
physicians and patients.
Public Health Reports, 112
(5), 410-7.
Institute of Medicine. (2001).
Crossing the quality chasm: A new system of health for the 21st century
.
Retrieved from http://www.nap.edu/openbook.php?isbn=0309072808

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Bibliography 39
Institute of Medicine. (2003).
Unequal treatment: Confronting racial and ethnic disparities in health care.
Retrieved from http://www.nap.edu/openbook.php?record_id=10260&page=R1
Institute of Medicine. (2004). In the Nation’s compelling interest: Ensuring diversity in the health care
workforce. Washington, DC: The National Academies Press.
Johnson, R.L., Saha, S., Arbelaez, Beach, M.C., & Cooper, L.A. (2004). Racial and ethnic differences in
patient perceptions of bias and cultural competence in health care. Journal of General Internal
Medicine, 19, 101-110.
The Joint Commission. (2010). Advancing effective communication, cultural competence, and patient-
and family-centered care: A roadmap for hospitals. Retrieved from
http://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf
Kairys, J., & Like, R.C. (2006). Caring for diverse populations: Do academic family medicine practices
have CLAS? Family Medicine, 38, 196-205.
Khanna, S. K., Cheyney, M., & Engle, M. (2009). Cultural competency in health care: Evaluating the
outcomes of a cultural competency training among health care professionals. Journal of the
National Medical Association, 101, 886–892.
Kleinman, A., Eisenberg, L., & Good, B. (1978). Culture, illness, and care: Clinical lessons from
anthropologic and cross-cultural research. Annals of Internal Medicine, 88, 251-258.
Kumagai, A.K., & Lypson, M.L. (2009). Beyond cultural competence: Critical consciousness, social justice,
and multicultural education. Academic Medicine, 84, 782-787.
LaVeist, T. A., Gaskin, D. J., & Richard, P. (2009). The economic burden of health inequalities in the
United States. Retrieved from the Joint Center for Political and Economic Studies website:
http://www.jointcenter.org/sites/default/files/upload/research/files/The%20Economic%20Burden
%20of%20Health%20Inequalities%20in%20the%20United%20States.pdf
Lie, D. A., Lee-Rey, E., Gomez, A., Bereknyel, S., & Braddock, C. H. (2010). Does cultural competency
training of health professionals improve patient outcomes? A systematic review and proposed
algorithm for future research. Journal of General Internal Medicine, 26(3), 317–325.
doi:10.1007/s11606-010-1529-0
McKirnan, D.J., DuBois, S.N., Alvy, L.M., & Jones, K. (2012). Health care access and health behaviors
among men who have sex with men: The cost of health disparities. Health Education and
Behavior. Advance online publication. doi:10.1177/1090198111436340
National Partnership for Action to End Health Disparities. (2011a). National stakeholder strategy for
achieving health equity. Retrieved from U.S. Department of Health and Human Services, Office of
Minority Health website:
http://www.minorityhealth.hhs.gov/npa/templates/content.aspx?lvl=1&lvlid=33&ID=286

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Bibliography 40
National Partnership for Action to End Health Disparities. (2011b). Toolkit for community action.
Retrieved from U.S. Department of Health and Human Services, Office of Minority Health
website: http://minorityhealth.hhs.gov/npa/files/Plans/Toolkit/NPA_Toolkit.pdf
Passel, J. S., & Cohn, D. (2008).
U.S. population projections: 2005-2050
. Retrieved from the Pew
Research Center website: http://pewsocialtrends.org/files/2010/10/85.pdf
Ross, L. (1995). The spiritual dimension: Its importance to patients’ health, well-being and quality of life
and its implication for nursing practice.
International Journal of Nursing Studies
,
32
(5), 457-468.
Saha, S., Beach, M. C., & Cooper, L. A. (2008). Patient centeredness, cultural competence, and
healthcare quality.
Journal of the National Medical Association
,
100
(11), 1275–1285. Retrieved
from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2824588/?tool=pubmed
Sperling, J. (2011).
Communicating more for less: Using translation and interpretation technology to
serve limited English proficient individuals
. Retrieved from the Migration Policy Institute website:
http://www.migrationpolicy.org/pubs/LEP-translationtechnology.pdf
Sue, D.W. (2001). Multidimensional facets of cultural competence.
The Counseling Psychologist, 29
(6),
790-821.
Sullivan, L.W., & Mittman, I.S. (2010). The state of diversity in the health professions a century after
Flexner.
Academic Medicine, 85
, 246-253.
The Patient Protection and Affordable Care Act, PL 111-148 (2010).
Thom, D., Hall, M., & Pawlson, G. (2004). Measuring patients’ trust in physicians when assessing quality
of care.
Health Affairs 23
(4), 124-132.
Thorson, J.A., & Cook, T.C. (1980).
Spiritual well-being of the elderly
. Springfield, IL: Charles C Thomas
Publisher Ltd.
Tseng, W.S., & Streltzer, J.M. (2008). Culture and medical practice. In W.S., Tseng & J.M. Streltzer
(eds.).
Cultural competence in health care
. (pp.1-12). New York: Springer.
U.S. Department of Commerce, Census Bureau. (2010).
American community survey
. Retrieved from
http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_10_3YR
_DP02&prodType=table
U.S. Department of Health and Human Services. (2011).
HHS action plan to reduce racial and ethnic
health disparities: A nation free of disparities in health and health care
. Retrieved from
http://minorityhealth.hhs.gov/npa/files/Plans/HHS/HHS_Plan_complete.pdf
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2012a).
National healthcare quality report
. (AHRQ Publication No. 12-0005). Retrieved from
http://www.ahrq.gov/qual/measurix.htm#quality

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Bibliography 41
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2012b).
National healthcare disparities report
. (AHRQ Publication No. 12-0006). Retrieved from
http://www.ahrq.gov/qual/measurix.htm#disparity
U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. (2011). CDC
Health disparities and inequalities report – United States, 2011.
MMWR, 60
, 1-109.
U.S. Department of Health and Human Services, Health Resources and Services Administration. (2005).
Transforming the face of health professions through cultural and linguistic competence
education: The role of the HRSA centers of excellence
. Retrieved from
http://www.hrsa.gov/culturalcompetence/cultcompedu.pdf
U.S. Department of Health and Human Services, Indian Health Services. (n.d.).
Our mission
. Retrieved
from http://www.ihs.gov/index.cfm?module=ihsIntro
U.S. Department of Health and Human Services, Office for Civil Rights. (2003).
Guidance to federal
financial assistance recipients regarding Title VI prohibition against national origin discrimination
affecting limited English proficient persons.
Retrieved from
http://www.hhs.gov/ocr/civilrights/resources/laws/revisedlep.html
U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion.
(2010a).
Healthy people 2020: Social determinants of health
. Retrieved from
http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=39
U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion.
(2010b).
Healthy people 2020
. Retrieved from http://www.healthypeople.gov/2020/default.aspx
U.S. Department of Health and Human Services, Office of Minority Health. (2005).
What is cultural
competency?
Retrieved from
http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlID=11
U.S. Department of Health and Human Services, Office of Minority Health (2011).
National partnership for
action to end health disparities
. Retrieved from http://minorityhealth.hhs.gov/npa
U.S. Department of Health and Human Services, Office of Minority Health, Think Cultural Health. (2012).
CLAS legislation map
. Retrieved from
https://www.thinkculturalhealth.hhs.gov/Content/LegislatingCLAS.asp
U.S. Department of Health and Human Services, Office of the Surgeon General and National Action
Alliance for Suicide Prevention. (2012).
2012
National strategy for suicide prevention: Goals and
objectives for action
. Retrieved from http://www.surgeongeneral.gov/library/reports/national-
strategy-suicide-prevention/full_report-rev.pdf
World Health Organization. (1946).
Definition of health in preamble to the constitution of the World
Health Organization
. Geneva, Switzerland: World Health Organization.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Bibliography 42
World Health Organization. (2012).
Social determinants of health
. Retrieved from
http://www.who.int/social_determinants/en/
Wilson-Stronks, A., & Galvez, E. (2007).
Hospitals, language, and culture: A snapshot of the nation.
Retrieved from The Joint Commission website:
http://www.jointcommission.org/assets/1/6/hlc_paper.pdf
Wynia, M. K., Johnson, M., McCoy, T. P., Passmore Griffin, L., & Osborn, C. Y. (2010). Validation of an
organizational communication climate assessment toolkit.
American Journal of Medical Quality,
25
(6), 436–443. doi:10.1177/1062860610368428
Youdelman, M. (2011).
The ACA and language access.
Retrieved from the National Health Law Program
website:
http://www.healthlaw.org/images/stories/Short_Paper_5_The_ACA_and_Language_Access.pdf
Youdelman, M., & Perkins, J. (2005).
Providing language services in small health care provider settings:
Examples from the field
(Commonwealth Fund Publication No. 810). Retrieved from The
Commonwealth Fund website:
http://www.commonwealthfund.org/usr_doc/810_Youdelman_providing_language_services.pdf
Zambrana, R.E., Molnar, C., Munoz, H.B., & Lopez, D.S. (2004). Cultural competency as it
intersects with racial/ethnic, linguistic, and class disparities in managed healthcare
organizations.
American Journal of Managed Care, 10
, SP37-SP44.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
The Blueprint 43
The Blueprint
The National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care: A
Blueprint for Advancing and Sustaining CLAS
offers a user-friendly format for providing comprehensive —
but by no means exhaustive — information on each Standard.
Each chapter is structured in the following manner:
Table 1: Blueprint Chapter Structure
Standard: Statement of the National CLAS Standard
Purpose:
A list of many of the Standard’s purposes to contextualize its intent and
importance
Components of the
Standard:
An explanation of the Standard’s elements to provide additional information on
the concepts presented
Strategies for
Implementation:
Practical recommendations on implementing each Standard in various
organizations or settings
Resources:
Seminal
documents and other relevant resources related to the Standard to
assist individuals and organizations in laying the foundation for CLAS
Bibliography: Documents cited within the Standard chapter
The HHS Office of Minority Health will also maintain a Web version of
The Blueprint
to provide a more
comprehensive and up-to-date resource. It is our hope that
The Blueprint
will aid in the adoption of the
enhanced National CLAS Standards in order to help advance better health and health care in the United
States.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 1 44
Standard 1: Provide Effective, Equitable, Understandable, and
Respectful Quality Care and Services
Standard 1
The National CLAS Standards are intended to advance health equity, improve quality, and help eliminate
health care disparities by establishing a blueprint for health and health care organizations to:
Provide effective, equitable, understandable, and respectful quality care and services that are responsive
to diverse cultural health beliefs and practices, preferred languages, health literacy, and other
communication needs.
Purpose
The purposes of providing effective, equitable, understandable, and respectful quality care and services
are:
o To create a safe and welcoming environment at every point of contact that both fosters
appreciation of the diversity of individuals and provides patient- and family-centered care
o To ensure that all individuals receiving health care and services experience culturally and
linguistically appropriate encounters
o To meet communication needs so that individuals understand the health care and services they
are receiving, can participate effectively in their own care, and make informed decisions
o To eliminate discrimination and disparities
Please refer to the glossary in Appendix A for definitions of the key terms used.
Components of the Standard
Effective, equitable, understandable, and respectful quality care and services
Effective care and services are those that successfully restore an individual to his/her desired health
status and help to protect his/her future health. An essential part of ensuring that care and services are
effective is to ensure that they are culturally and linguistically appropriate (IOM, 2003). All health care
and services should be culturally and linguistically appropriate, including but not limited to health
promotion, disease prevention, diagnosis, treatment, supportive care, rehabilitation, palliative end-of-life
care, mental and behavioral health, emergency care, and wellness interventions. Vital to the provision of

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 1 45
effective health care and services, providers must accurately understand the issue or illness, determine
the course of treatment or services for that individual, and negotiate the solution or treatment
successfully with the individual. Cultural and linguistic competency allows providers to navigate the
cultural and linguistic factors that affect trust, rapport, communication, and adherence (Ngo-Metzger et
al., 2006).
Equitable care and services must apply to all individuals and groups regardless of their cultural
identity or identities. The aim of equitable care and services is to reduce the burden of illness, injury, and
disability and to improve the health and functioning of all people in the United States (IOM, 2001). Equity
is a key component of quality care (National Quality Forum, 2009). Equitable care and services are
influenced by a number of factors, including but not limited to race, education, health literacy, age,
sexual orientation, ethnicity, religion, physical or mental disability, language, gender, gender expression,
gender identity, income, class, and access to care (California Pan-Ethnic Health Network, 2010; National
Partnership for Action to End Health Disparities, 2011). The Joint Commission states in
Advancing
Effective Communication, Cultural Competence, and Patient- and Family-Centered Care: A Roadmap for
Hospitals
that all individuals have the right to be free of discrimination while accessing care or services,
whether or not that is included in the specific state’s laws and regulations (The Joint Commission, 2010).
Understandable care and services rely on a clear exchange of information between those providing
care and services and those receiving them. Individuals should be able to fully comprehend how to
access care and services, what their treatment options are, and what they need to get and stay well.
Ensuring that care and services are understandable is particularly important to those who have limited
English proficiency, are deaf or hard of hearing, or may have difficulty comprehending the health care
system and its terminology. It is estimated that nearly 90% of adults have difficulty using everyday
health information routinely found in health care facilities, retail outlets, media, and communities. Such
estimates highlight the significance of ensuring that health care and services are understandable since
limited health literacy is associated with, among other factors, poorer health outcomes and higher health
care costs (HHS ODPHP, 2012). See also Health Literacy section of this chapter.
Respectful care and services are important to fostering an environment in which individuals from
diverse backgrounds will feel comfortable discussing their needs with any member of an organization’s
staff. The HHS Consumer Bill of Rights states that all recipients of services have “the right to considerate,
respectful care from all members of the health care system at all times and under all circumstances”
(Advisory Commission on Consumer Protection and Quality in the Health Care Industry, 1997, Chapter 5,
para. 1).
Accordingly, all members of the health and health care team should:
o Provide individuals with assurances that disrespect or discrimination of any kind is intolerable

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 1 46
o Provide individuals with reasonable assistance to overcome language, cultural, physical, or
communication barriers
Cultural Health Beliefs and Practices
The integrated pattern of thoughts, communications, actions, beliefs, values, and institutions associated
with one’s cultural identity informs how individuals perceive illness, its cause, its treatment, and what
wellness may look like (Horky et al., n.d.). Cultural beliefs and practices also influence how individuals
cope with chronic or terminal illnesses. Health professionals should understand and be aware of the role
that cultural health beliefs and practices play in their own lives as well as the lives of the individuals
seeking services.
A commitment to lifelong learning is an intrinsic value to many in the fields of health and health care
(Association of American Medical Colleges and American Association of the Colleges of Nursing, 2010;
American Physical Therapy Association, 2012; American Public Health Association, n.d.). It is incumbent
upon providers and staff members to include in their lifelong learning an ongoing commitment to self-
reflection and honest self-assessment in order to understand how their own cultural beliefs inform their
daily lives and professional activities (Tervalon & Murray-Garcia, 1998). It is through continued self-
assessment and awareness of others’ cultural beliefs that mutually beneficial relationships between
provider and individual, and between organization and community, may be cultivated.
Providers and staff should inquire about and understand the healing practices and health regimens,
including traditional healer services, used by the individuals they serve and integrate these approaches
into treatment plans when appropriate. In the pursuit to learn about the various cultural beliefs and
health practices in their communities, providers and staff should, whenever possible, gather this
information directly from the individual seeking care or services. Through this awareness, the provider
will be able to negotiate treatment options in a culturally and linguistically appropriate manner (American
Institutes for Research, 2002). As providers and staff learn about the cultural health beliefs and practices
of different communities, it is important that this knowledge not be used to stereotype or overgeneralize
(Tervalon & Murray-Garcia, 1998).
Preferred Languages
In the United States, over 24 million people (8.7% of the population) speak English less than very well
(U.S. Census Bureau, 2010) and should be considered limited English proficient for health and health care
purposes, according to The Joint Commission’s
Advancing Effective Communication, Cultural
Competence, and Patient- and Family-Centered Care: A Roadmap for Hospitals
(2010). In addition,
individuals who are conversant in English may not adequately comprehend the complexities of health and
medical discussions in English. Health professionals should determine the communication and language
assistance needed for individuals with limited English proficiency, including interpreters, translated

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 1 47
materials, signage and wayfinding. Furthermore, communication should reflect an appropriate health
literacy level. According to the Roadmap for Hospitals, it is also critical to remember that someone who
speaks English may not be able to read it (The Joint Commission, 2010). See also Understandable Care
and Services and Health Literacy sections of this chapter.
Health Literacy
Health literacy is the degree to which an individual has the capacity to obtain, process, and understand
basic health information and services needed to make appropriate health decisions (HHS ODPHP, 2000).
The majority of American adults have limited ability to be active participants and decision-makers when it
comes to their health and health care needs.
o Only 12% of adults have proficient health literacy, meaning nearly 9 out of 10 adults may lack
the skills needed to manage their health and prevent disease (Kutner, Greenburg, Jun, &
Paulsen, 2006).
o Adults with limited literacy skills are less likely to manage their chronic diseases and more likely
to be hospitalized than adults with stronger literacy skills. This leads to poorer health outcomes
and higher health care costs (Berkman, Sheridan, Donahue, Halpern, & Crotty, 2011).
o There is a mismatch between the communication needs of the public and the communication
level of professionals in the fields of health and human services. The complexity of health
information and the health care delivery system affect an individual’s ability to understand and
use health information. A better match between the health literacy level of the population served
and the health literacy level of the information communicated results in improved
communication, greater adherence to treatment, greater ability to engage in self-care, improved
health status, and greater efficiency and cost savings to the health system as a whole (HHS
ODPHP, 2010).
The HHS Agency for Healthcare Research and Quality has developed a toolkit that outlines health literacy
universal precautions, defined as “actions that minimize risk for everyone when it is unclear which
patients may be affected” by low health literacy. Universal precautions are necessary because health
professionals cannot always identify individuals with low health literacy (AHRQ, 2010) (see Standard 8).
Communication Needs
Individuals frequently report that health professionals are not meeting their communication needs. Racial
and ethnic minorities, individuals with limited English proficiency, and those with less education are more
likely to have communication difficulties and to rate health care communication poorly (Wynia &
Matiasek, 2006).
Communication needs of some individuals may be easily recognized, while others may
be more difficult to discern (Wynia & Matiasek, 2006). According to The Joint Commission’s
Advancing
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 1 48
Effective Communication, Cultural Competence, and Patient- and Family-Centered Care: A Roadmap for
Hospitals
, organizations should provide communication and language assistance to include interpreters,
translated materials, signage and wayfinding, augmentative and alternative communication resources,
and auxiliary aids and services (The Joint Commission, 2010). See Standards 5, 6, 7, and 8 and the
Glossary for additional information and guidance.
Strategies for Achievement of the Principal Standard
Standard 1 is the Principal Standard because, conceptually, the ultimate aim in adopting the remaining
Standards is to achieve Standard 1. Standards 2 through 15 represent the practices and policies intended
to be the fundamental building blocks of culturally and linguistically appropriate services that are
necessary to achieve the Principal Standard. For this reason, Strategies for Implementation specific to
Standard 1 are not listed here. If each of Standards 2 through 15 is implemented and maintained,
organizations will be better positioned to achieve the desired goal of “effective, equitable,
understandable, and respectful quality care and services that are responsive to diverse cultural health
beliefs and practices, preferred languages, health literacy, and other communication needs.”
Resources
American Medical Association. (2006). Improving communication, improving care: How health care
organizations can ensure effective, patient-centered communication with people from diverse
populations. Retrieved from http://www.ama-assn.org/resources/doc/ethics/pcc-consensus-
report.pdf
Health Research & Educational Trust, Institute for Diversity in Health Management (2011). Building a
culturally competent organization: The quest for equity in health care. Retrieved from
http://www.hret.org/quality/projects/resources/cultural-competency.pdf
National Patient Safety Foundation. (n.d.). Ask me 3. Retrieved from http://www.npsf.org/for-healthcare-
professionals/programs/ask-me-3
Pfizer. (2011). Prevalence calculator. Retrieved from http://www.pfizerhealthliteracy.com/physicians-
providers/PrevalenceCalculator.aspx
Saha, S., Beach, M. C., & Cooper, L. A. (2008). Patient centeredness, cultural competence and healthcare
quality. Journal of the National Medical Association, 100(11), 1275–1285. Retrieved from
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2824588
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2010).
Health literacy universal precautions toolkit (AHRQ Publication No. 10-0046-EF). Retrieved from
http://www.ahrq.gov/qual/literacy/
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 1 49
U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion.
(2010). National action plan to improve health literacy. Retrieved from
http://www.health.gov/communication/HLActionPlan/pdf/Health_Literacy_Action_Plan.pdf
Wynia, M., & Matiasek, J. (2006). Promising practices for patient-centered communication with vulnerable
populations: Examples from eight hospitals (Commonwealth Fund Publication No. 947). Retrieved
from The Commonwealth Fund website:
http://www.commonwealthfund.org/~/media/Files/Publications/Fund%20Report/2006/Aug/Promi
sing%20Practices%20for%20Patient%20Centered%20Communication%20with%20Vulnerable%
20Populations%20%20Examples%20from%20Ei/Wynia_promisingpracticespatientcentered_947
%20pdf.pdf
Additional resources can be found in Appendix E and at www.ThinkCulturalHealth.hhs.gov.
Bibliography
Advisory Commission on Consumer Protection and Quality in the Health Care Industry. (1997).
Consumer
bill of rights and responsibilities: Report to the president of the United States.
Retrieved from
http://www.opm.gov/insure/archive/health/cbrr.htm
Association of American Medical Colleges and American Association of the Colleges of Nursing. (2010).
Lifelong learning in medicine and nursing: Final conference report
. Retrieved from
https://www.aamc.org/download/121492/data/macyreport2010.pdf.pdf
American Institutes for Research. (2002).
Teaching cultural competence in health care: A review of
current concepts, policies and practices
. Retrieved from Office of Minority Health website:
http://minorityhealth.hhs.gov/assets/pdf/checked/1/em01garcia1.pdf
American Physical Therapy Association. (2012).
Professional development, lifelong learning, and
continuing competence in physical therapy
. Retrieved from
http://www.apta.org/uploadedFiles/APTAorg/About_Us/Policies/HOD/Professional_Development/
ProfessionalDev.pdf
American Public Health Association. (n.d.).
The education board
. Retrieved from
http://www.apha.org/about/gov/edboard/
Berkman, N. D., Sheridan, S. L., Donahue, K. E., Halpern, D. J., & Crotty, K. (2011). Low health literacy
and health outcomes: An updated systematic review.
Annals of Internal Medicine, 155
(2), 97–
107.
California Pan-Ethnic Health Network. (2010).
Building quality & equitable health care systems.
(Conference
report). Retrieved from
http://www.cpehn.org/pdfs/Building%20Quality%20and%20Equitable%20Health%20Care%20Sy
stems%2010-10.pdf

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 1 50
Horky, S., Tribby, R., Becker, C., Phipps, M. J., Saperstein, M., Johnston, J., & Polanco, B.-P. (n.d.). Core
concepts in cultural competence: Health beliefs. In
Cross-cultural health care: Case studies
.
Retrieved from http://support.mchtraining.net/national_ccce/case0/concepts.html#4
Institute of Medicine. (2001).
Crossing the quality chasm: A new system of health for the 21st century
.
Retrieved from http://www.nap.edu/openbook.php?isbn=0309072808
Institute of Medicine. (2003).
Unequal treatment: Confronting racial and ethnic disparities in health care.
Retrieved from http://www.nap.edu/openbook.php?record_id=10260&page=R1
The Joint Commission. (2010).
Advancing effective communication, cultural competence, and patient-
and family-centered care: A roadmap for hospitals.
Retrieved from
http://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf
Kutner, M., Greenberg, E., Jin, Y., & Paulsen, C. (2006).
The health literacy of America’s adults: Results
from the 2003 National Assessment of Adult Literacy
(NCES 2006–483). Washington, DC:
National Center for Education Statistics.
National Partnership for Action to End Health Disparities. (2011).
National stakeholder strategy for
achieving health equity: Development of the national stakeholder strategy.
Retrieved from U.S.
Department of Health and Human Services, Office of Minority Health website:
http://minorityhealth.hhs.gov/npa/files/Plans/NSS/NSS_05_Section1.pdf
National Quality Forum. (2009).
A comprehensive framework and preferred practices for measuring and
reporting cultural competency: A consensus report.
Retrieved from
http://www.qualityforum.org/Publications/2009/04/A_Comprehensive_Framework_and_Preferred
_Practices_for_Measuring_and_Reporting_Cultural_Competency.aspx
Ngo-Metzger, Q., Telfair, J., Sorkin, D. H., Weidmer, B., Weech-Maldonado, R., Hurtado, M., & Hays, R.
D. (2006).
Cultural competency and quality of care: Obtaining the patient’s perspective
. Retrieved
from The Commonwealth Fund website: http://www.commonwealthfund.org/usr_doc/Ngo-
Metzger_cultcompqualitycareobtainpatientperspect_963.pdf
Tervalon, M., & Murray-Garcia, J. (1998). Cultural humility versus cultural competence: A critical
distinction in defining physician training outcomes in multicultural education.
Journal of Health
Care for the Poor and Underserved, 9
(2), 117–125.
U.S. Department of Commerce, Census Bureau. (2010).
American community survey.
Retrieved from
http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_10_3YR
_DP02&prodType=table
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2010).
Health literacy universal precautions toolkit
(AHRQ Publication No. 10-0046-EF). Retrieved from
http://www.ahrq.gov/qual/literacy/
U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion.
(2000). Health communication and health IT. In
Healthy people 2010
. Retrieved from

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 1 51
http://www.healthypeople.gov/2010/hp2020/Objectives/TopicArea.aspx?id=25&TopicArea=Healt
h+Communication+and+Health+IT
U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion.
(2010).
National action plan to improve health literacy.
Retrieved from
http://www.health.gov/communication/HLActionPlan/pdf/Health_Literacy_Action_Plan.pdf
U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion.
(2012).
Health literacy.
Retrieved from http://www.health.gov/communication/literacy
Wynia, M., & Matiasek, J. (2006).
Promising practices for patient-centered communication with vulnerable
populations: Examples from eight hospitals
(Commonwealth Fund Publication No. 947). Retrieved
from The Commonwealth Fund website:
http://www.commonwealthfund.org/~/media/Files/Publications/Fund%20Report/2006/Aug/Promi
sing%20Practices%20for%20Patient%20Centered%20Communication%20with%20Vulnerable%
20Populations%20%20Examples%20from%20Ei/Wynia_promisingpracticespatientcentered_947
%20pdf.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 2 52
Standard 2: Advance and Sustain Governance and Leadership that
Promotes CLAS and Health Equity
Standard 2
The National CLAS Standards are intended to advance health equity, improve quality, and help eliminate
health care disparities by establishing a blueprint for health and health care organizations to:
Advance and sustain organizational governance and leadership that promotes CLAS and health equity
through policy, practices, and allocated resources.
Purpose
The purposes of advancing and sustaining governance and leadership that promotes CLAS and health
equity are:
o To ensure the provision of appropriate resources and accountability needed to support and
sustain initiatives
o To model an appreciation and respect for diversity, inclusiveness, and all beliefs and practices
o To support a model of transparency and communication between the service setting and the
populations that it serves
Please refer to the glossary in Appendix A for definitions of the key terms used.
Components of the Standard
Advance and sustain organizational governance and leadership that promotes CLAS and
health equity
Standard 2 is a new Standard that resulted from the National CLAS Standards Enhancement Initiative.
Standard 2 has been added to underscore that CLAS must permeate every aspect of the organization,
from the top down and from the bottom up. Cultural and linguistic competency has historically been a
grassroots strategy. However, it is the organization’s leadership that establishes the culture of the
organization through its priorities, expectations, and the behavior that it models (Schyve & The
Governance Institute, 2009) and through designing service delivery processes and expectations (Rice,
2007).

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 2 53
Health and health care governance and leadership bodies should make their commitment to CLAS highly
visible to both staff and individuals in their service area (Wilson-Stronks & Galvez, 2007). Leadership, in
large part, determines whether the organization’s culture will embody quality, safety, and CLAS (Schyve
& The Governance Institute, 2009), so much so that diversity in leadership has been found to be the
single most significant predictor of adoption and adherence to the National CLAS Standards (Weech-
Maldonado, 2007). This may be because support from governance and leadership enables the allocation
of resources and services necessary to effectively and efficiently meet individual or group communication,
cultural, religious, spiritual, mobility, and other needs, according to The Joint Commission’s
Advancing
Effective Communication, Cultural Competence, and Patient- and Family-Centered Care: A Roadmap for
Hospitals
(2010).
The Health Research and Educational Trust, an affiliate of the American Hospital Association, poses two
key questions for organizational leadership in regard to prioritizing cultural competency (HRET, 2011):
1. Has your board set goals on improving organizational diversity, providing culturally competent
care, and eliminating disparities in care as part of your strategic plan?
2. Is diversity awareness and cultural competency training mandatory for all senior leadership,
management, staff, and volunteers?
These two questions are directly related to enhanced National CLAS Standards 8 and 3, respectively, and
emphasize that the key strategy for embedding CLAS within an organization is engaging leadership.
Indeed, research has shown leadership commitment as one of the most significant elements for
integrating cultural and linguistic competency and moving CLAS from theory to action (HHS OMH, 2004;
Weech-Maldonado, 2007; Wu & Martinez, 2006). A multi-stakeholder expert panel convened by the
American Medical Association and Health Research and Educational Trust in 2006 called on all health care
organizations to regularly assess “leadership involvement; mission, goals and strategies; policies and
programs; budget allocations; and workforce values” as they relate to culturally and linguistically
appropriate services (AMA, 2006, pp. 28–32). In one study, patients at hospitals and clinics that scored
just 5 points higher (out of 100) on a domain measuring resource allocation and leadership engagement
in addressing CLAS were more likely to report receiving high-quality care and more likely to report high
levels of trust in the organization, compared to those who scored lower (Wynia et al., 2010).
Furthermore, the National Quality Forum identifies leadership as one of the seven primary domains for
measuring and reporting cultural competency.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 2 54
“Leadership recognizes that healthcare providers, clinical and organizational leaders, the governance
board, and the community share responsibility for and play an essential role in the development and
implementation of cultural competency activities, in setting policy and strategy and in monitoring
organization performance. Leadership must aspire to reflect the diversity of the community served.”
(National Quality Forum, 2009, p. iv)
Promote CLAS and health equity through policy, practices, and allocated resources
Organizational governance and leadership play a key role in promoting CLAS and health equity through
policies, practices, and resource allocation. Institutionalizing cultural competency into organizations’
central missions; collecting race, ethnicity, and primary language data; and increasing the diversity of the
leadership, governance, and workforce within the organization represent methods that leaders should use
to improve equity, quality, and efficacy of services (HRET, 2011). The following table illustrates how a
few prominent health and health care organizations promote CLAS and health equity; namely, through
policies and practices described in their mission, vision, and/or values statements. While certainly not
exhaustive, the examples listed illustrate how several organizations have sought to address these topics.
Table 2: Examples of Promoting CLAS Through Policy and Practice
Association URL Mission/Vision/Core Values
American Public
Health Association
http://www.apha.org/a
bout/gov/execboard/ex
ecutiveboardvisionmissi
on.htm
Mission:
Improve the health of the public and achieve equity in
health status
Johns Hopkins
Medicine
http://www.hopkinsme
dicine.org/about/missio
n.html
Mission:
The mission of Johns Hopkins Medicine is to improve
the health of the community and the world by setting the
standard of excellence in medical education, research, and
clinical care. Diverse and in
clusive, Johns Hopkins Medicine
educates medical students, scientists, health care professionals,
and the public; conducts biomedical research; and provides
patient-centered medicine to prevent, diagnose, and treat human
illness.
Vision:
Johns Hopkins Medicine provides a diverse and inclusive
environment that fosters intellectual discovery, creates and
transmits innovative knowledge, improves human health, and
provides medical leadership to the world.
Core Values:
Excellence and Discovery, Leadership and
Integrity, Diversity and Inclusion, Respect and Collegiality
Harvard Medical
School
http://hms.harvard.edu
/hms/facts.asp
Mission:
To create and nurture a diverse community of the best
people committed to leadership in alleviating human suffering
caused by disease.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 2 55
Association URL Mission/Vision/Core Values
Mayo Clinic
http://www.mayoclinic.
org/about/missionvalue
s.html
Mission:
To inspire hope and contribute to health and well-
being by providing the best care to every patient through
integrated clinical practice, education, and research.
Values:
These values, which guide Mayo Clinic's mission to this
day, are an expression of the vision and intent of our founders,
the original Mayo physicians, and the Sisters of Saint Francis.
o
Respect:
Treat everyone in our diverse community,
including patients, their families, and colleagues, with
dignity.
o
Compassion:
Provide the best care, treating patients and
family members with sensitivity and empathy.
o
Integrity:
Adhere to the highest standards of
professionalism, ethics, and personal responsibility, worthy
of the trust our patients place in us.
o
Healing:
Inspire hope and nurture the well-being of the
whole person, respecting physical, emotional, and spiritual
needs.
o
Teamwork:
Value the contributions of all, blending the
skills of individual staff members in unsurpassed
collaboration.
o
Excellence:
Deliver the best outcomes and highest quality
service through the dedicated effort of every team
member.
o
Innovation:
Infuse and energize the organization,
enhancing the lives of those we serve, through the creative
ideas and unique talents of each employee.
o
Stewardship:
Sustain and reinvest in our mission and
extended communities by wisely managing our human,
natural, and material resources.
Society of Public
Health Educators
http://www.sophe.org/
mission.cfm
Values:
The Society of Public Health Educators is committed
to:
o Responding to the needs of its members
o Delivering quality products and services
o Demonstrating integrity, accountability and transparency
o Promoting teamwork and collaboration
o Embracing diversity
o Respecting organizational tradition while encouraging
innovation
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 2 56
In addition, Johns Hopkins Medicine recently adopted a multiyear strategic plan, entitled Diversity &
Inclusion 2020
,
which establishes key goals for patient care, community engagement and involvement,
and workforce development. In implementing this strategic plan, the organization established an Office of
Diversity and Cultural Competence and appointed an Associate Dean of Diversity and a diversity
specialist, and to develop e-learning courses on diversity and cultural competency issues in conjunction
with the School of Public Health’s Center for Health Disparities Solutions. The hospital has developed
partnerships with the community to foster increased diversity and community engagement (Johns
Hopkins Medicine, n.d.).
Strategies for Implementation
The following are possible implementation strategies for advancing and sustaining governance and
leadership that promotes CLAS and health equity:
From the National Quality Forum (2009):
o Create and sustain an environment of cultural competency through establishing leadership
structures and systems or embedding them into existing structures and systems.
o Identify and develop informed and committed champions of cultural competency throughout the
organization in order to focus efforts around providing culturally competent care.
o Ensure that a commitment to culturally competent care is reflected in the vision, goals, and
mission of the organization and couple this with an actionable plan.
o Implement strategies to recruit, retain, and promote at all levels of the organization a diverse
leadership that reflects the demographic characteristics of the populations in the service area.
o Ensure that the necessary fiscal and human resources, tools, skills, and knowledge to support
and improve culturally competent policies and practices in the organization are available.
o Commit to cultural competency through system-wide approaches that are articulated through
written policies, practices, procedures, and programs.
o Actively seek strategies to improve the knowledge and skills that are needed to address cultural
competency in the organization.
From The Joint Commission (Wilson-Stronks & Galvez, 2007):
o Provide for internal multidisciplinary dialogues about language and culture issues.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 2 57
o Create financial incentives to promote, develop, and maintain accessibility to qualified health care
interpreters.
Resources
American Medical Association. (2006). Content area 1. Understand your organization’s commitment. In
Improving communication, improving care: How health care organizations can ensure effective,
patient-centered communication with people from diverse populations (pp. 28–32). Retrieved
from http://www.ama-assn.org/resources/doc/ethics/pcc-consensus-report.pdf
Betancourt, J., Green, A., & King, R. (2008). Improving quality and achieving equity: A guide for hospital
leaders. Retrieved from Massachusetts General Hospital, The Disparities Solutions Center
website:
http://www2.massgeneral.org/disparitiessolutions/z_files/disparities%20leadership%20guide_fina
l.pdf
Georgetown University Child Development Center, Center for Child Health and Mental Health Policy,
National Center for Cultural Competence. (2000). A planner's guide: Infusing principles, content
and themes related to cultural and linguistic competence into meetings and conferences.
Retrieved from http://gucchd.georgetown.edu/products/PlannersGuide.pdf
Institute for Diversity in Health Management. (2004). Strategies for leadership: Does your hospital reflect
the community it serves? Diversity and cultural proficiency assessment tool for leaders. Retrieved
from http://www.aha.org/content/00-10/diversitytool.pdf
Institute for Diversity in Health Management. (2008). Institute Resource Center. Retrieved from
http://www.diversityconnection.org/diversityconnection/membership/Institute-Resource-
Center.jsp?fll=S12
Liteman, M., Campbell, S., & Liteman, J. (2006). Retreats that work: Everything you need to know about
planning and leading great offsites. San Francisco, CA: Pfeiffer.
Management Sciences for Health. (n.d.). The provider’s guide to quality & culture. Retrieved from
http://erc.msh.org/mainpage.cfm?file=1.0.htm&module=provider&language=English
Powell, L., & Taylor, C. (2004). Hospital governing board assessment: A self-help guide. Boise, ID:
Mountain States Group.
Schyve, P. M., & The Governance Institute. (2009). Leadership in healthcare organizations: A guide to
Joint Commission leadership standards. Retrieved from
http://www.jointcommission.org/assets/1/18/WP_Leadership_Standards.pdf
Additional resources can be found in Appendix E and at www.ThinkCulturalHealth.hhs.gov.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 2 58
Bibliography
American Medical Association. (2006). Content area 1. Understand your organization’s commitment. In
Improving communication, improving care: How health care organizations can ensure effective,
patient-centered communication with people from diverse populations (pp. 28–32). Retrieved
from http://www.ama-assn.org/resources/doc/ethics/pcc-consensus-report.pdf
Health Research & Educational Trust, Institute for Diversity in Health Management (2011). Building a
culturally competent organization: The quest for equity in health care. Retrieved from
http://www.hret.org/quality/projects/resources/cultural-competency.pdf
Johns Hopkins Medicine. (n.d.). Diversity & inclusion 2020. Retrieved from
http://www.hopkinsmedicine.org/bin/s/x/diversity_and_inclusion.pdf
The Joint Commission. (2010). Advancing effective communication, cultural competence, and patient-
and family-centered care: A roadmap for hospitals. Retrieved from
http://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf
National Quality Forum. (2009). A comprehensive framework and preferred practices for measuring and
reporting cultural competency: A consensus report. Retrieved from
http://www.qualityforum.org/Publications/2009/04/A_Comprehensive_Framework_and_Preferred
_Practices_for_Measuring_and_Reporting_Cultural_Competency.aspx
Rice, M. F. (2007). Promoting cultural competency in public administration and public service delivery:
Utilizing self-assessment tools and performance measures. Journal of Public Affairs Education, 13,
41–57.
Schyve, P. M., & The Governance Institute. (2009). Leadership in healthcare organizations: A guide to
Joint Commission leadership standards. Retrieved from
http://www.jointcommission.org/assets/1/18/WP_Leadership_Standards.pdf
U.S. Department of Health and Human Services, Office of Minority Health. (2004). CLAS in health care:
Implementation of the National Standards for Culturally and Linguistically Appropriate Services in
Health Care at the Alameda Alliance for Health. Retrieved from
http://minorityhealth.hhs.gov/assets/pdf/checked/CLAS_healthcare.pdf
Weech-Maldonado, R. (2007, June). Moving towards culturally competent health systems: Organizational
and market factors. Presented at the AcademyHealth Disparities Interest Group Meeting,
Orlando, FL. Retrieved from
http://www.academyhealth.org/files/interestgroups/disparities/weech-maldonador.pdf
Wilson-Stronks, A., & Galvez, E. (2007). Hospitals, language, and culture: A snapshot of the nation.
Retrieved from The Joint Commission website:
http://www.jointcommission.org/assets/1/6/hlc_paper.pdf

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 2 59
Wu, E., & Martinez, M. (2006). Taking cultural competency from theory to action (Commonwealth Fund
Publication No. 964). Retrieved from The Commonwealth Fund website:
http://www.commonwealthfund.org/usr_doc/Wu_takingcultcomptheoryaction_964.pdf
Wynia, M. K., Johnson, M., McCoy, T. P., Passmore Griffin, L., & Osborn, C. Y. (2010). Validation of an
organizational communication climate assessment toolkit. American Journal of Medical Quality,
25(6), 436–443. doi:10.1177/1062860610368428
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 3 60
Standard 3: Recruit, Promote, and Support a Diverse Governance,
Leadership, and Workforce
Standard 3
The National CLAS Standards are intended to advance health equity, improve quality, and help eliminate
health care disparities by establishing a blueprint for health and health care organizations to:
Recruit, promote, and support a culturally and linguistically diverse governance, leadership, and
workforce that are responsive to the population in the service area.
Purpose
The purposes of recruiting, promoting, and supporting a diverse governance, leadership, and workforce
are:
o To create an environment in which culturally diverse individuals feel welcomed and valued
o To promote trust and engagement with the communities and populations served
o To infuse multicultural perspectives into planning, design, and implementation of CLAS
o To ensure diverse viewpoints are represented in governance decisions
o To increase knowledge and experience related to culture and language among staff
Please refer to the glossary in Appendix A for definitions of the key terms used.
Components of the Standard
Recruit, promote, and support a culturally and linguistically diverse governance, leadership,
and workforce
It is essential that organizations develop focused strategies to recruit, promote, and support a culturally
and linguistically diverse governance, leadership, and workforce. Evidence suggests that organizations
with a more diverse and better-trained workforce provide higher-quality care and experience greater
patient satisfaction scores (The Sullivan Commission on Diversity in the Healthcare Workforce, 2004;
IOM, 2003). For example, in one study, organizations scoring higher on a scale of workforce diversity and
training had better odds of patients reporting that they received high-quality care (Wynia et al., 2010).

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 3 61
Diversity should be present throughout every level of the organization, from front office personnel to the
senior leadership. Organizations and their staff should understand that diversity in governance,
leadership, and the workforce is about ensuring that individuals holding any organizational position
possess the necessary skills and qualifications to perform required duties. In addition, it should be
recognized that simply hiring and retaining a culturally diverse governance, leadership, and workforce is
not, by itself, sufficient to achieving culturally and linguistically appropriate services; all members of the
organization must be appropriately trained and versed in basic cultural competency skills (Rose, 2011;
Whealin & Ruzek, 2008). Supporting cultural diversity via recruitment, retention, and promotion is but
one method to ensure, among other things, that the opportunity for provider-patient concordance exists
and that the organizational culture is informed from a variety of perspectives (Smedley & Mittman, 2011).
Governance, leadership, and workforce that are responsive to the population in the service
area
The United States is rapidly becoming a more diverse nation. Since the 2000 U.S. Census, the percentage
of individuals identifying as either Hispanic or Asian has increased substantially (U.S. Census Bureau,
2011). It is projected that by 2050 the U.S. demographic makeup will be 47% White, 29% Hispanic, 13%
Black and 9% Asian (Passel & Cohn, 2008). This diversity, however, is not represented within many of
the health professions. Evidence indicates that an increase in racial and ethnic diversity among health
professionals is associated with increased access to care for racial and ethnic minority patients, greater
patient choice, more patient satisfaction and patient engagement, improved communication, and
improved educational experiences for health students (Cooper & Powe, 2004; IOM, 2004). Being
responsive to the community is important at all levels of the organization, including in the provision of
care and services, strategic planning, evaluation, and decision-making (Cooper & Powe, 2004).
Diversity among staff providing direct services in support, outreach, or clinical roles is important but not
sufficient. Though there may be a lack of diversity within certain health professions, organizations should
still strive to increase diversity throughout the entire hierarchy of an organization, including among senior
management, chief executives, and boards of directors. This can promote strategic planning as well as
policymaking and decision-making that are inclusive of the cultural and linguistic needs of all individuals
(HHS Health Resources and Services Administration, 2006). Governance, leadership, and a workforce that
is representative of the diversity of the communities served are motivating forces to make the
organization’s services increasingly relevant and effective for its constituents (U.S. Department of
Commerce, 1999).
Responsive care should also apply across various contractual relationships. Many health care
organizations use networks or affiliated providers to deliver services to their constituents. It is important
that staff diversity encompasses all individuals involved in health care delivery, whatever their contractual
or subcontractual relationship with the organization.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 3 62
Strategies for Implementation
The following are possible implementation strategies for the recruitment, promotion, and support of a
diverse governance, leadership, and workforce:
Recruitment
o Advertise job opportunities in targeted foreign language and minority health professional
associations’ job boards, publications, and other media (e.g., social media networks, professional
organizations’ email Listservs, etc.), and post information in multiple languages (QSource, 2005).
o Develop relationships with local schools, training programs, and faith-based organizations to
expand recruitment base (QSource, 2005).
o Recruit at minority health fairs (QSource, 2005).
o Collaborate with businesses, public school systems, and other stakeholders to build potential
workforce capacities and recruit diverse staff. In particular, linkages between academic and
service settings can help identify potential recruits already in the educational “pipeline” and
provide them with additional academic support and resources necessary to meet job
requirements (The Sullivan Commission on Diversity in the Healthcare Workforce, 2004).
o Assess the language and communication proficiency of staff to determine fluency and
appropriateness for serving as interpreters.
Promotion and Support
The Joint Commission’s
Advancing Effective Communication, Cultural Competence, and Patient- and
Family-Centered Care: A Roadmap for Hospitals
(2010) provides the following implementation strategies
for the promotion and support of a diverse governance, leadership, and workforce:
o Create a work environment that respects and accommodates the cultural diversity of the local
workforce.
o Develop, maintain, and promote continuing education and career development opportunities so
all staff members may progress within the organization.
o Cultivate relationships with organizations and institutions that offer health and human service
career training to establish volunteer, work-study, and internship programs.
Other strategies for promoting and supporting a diverse governance, leadership, and workforce include
(HHS OMH, 2001):
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 3 63
o Promote mentoring opportunities.
o Conduct regular, explicit assessments of hiring and retention data, current workforce
demographics, promotion demographics, and community demographics.
o Monitor work assignments and hire sufficient personnel to ensure a manageable and appropriate
workload for bilingual/bicultural staff members.
o Use nonclinical support staff in cultural broker positions only after providing sufficient training
and recognition (e.g., compensation, job title, or description).
o Promote diverse staff members into administrative or managerial positions where their cultural
and linguistic capabilities can make unique contributions to planning, policy, and decision-making.
o Foster an environment in which differences are respected and that is responsive to the
challenges a culturally and linguistically diverse staff brings into the workplace.
Resources
American Medical Association, The Ethical Force Program. (2006). Content area 4. Develop workforce. In
Improving communication—improving care: How health care organizations can ensure effective,
patient-centered communication with people from diverse populations (pp. 47–54). Retrieved
from http://www.ama-assn.org/resources/doc/ethics/pcc-consensus-report.pdf
American Medical Association. (2012). C-CAT: Patient centered communication. Retrieved from
http://www.ama-assn.org\go\ccat
Institute for Diversity in Health Management. (2004). Strategies for leadership: Does your hospital reflect
the community it serves? Diversity and cultural proficiency assessment tool for leaders. Retrieved
from http://www.aha.org/content/00-10/diversitytool.pdf
Smedley, B. D., Stith-Butler, A., & Bristow, L. R. (2004). In the nation’s compelling interest: Ensuring
diversity in the health-care workforce. Retrieved from
http://www.nap.edu/openbook.php?record_id=10885&page=1
The Sullivan Commission on Diversity in the Healthcare Workforce. (2004). Missing persons: Minorities in
the health professions. Retrieved from http://www.aacn.nche.edu/media-
relations/SullivanReport.pdf
Wynia, M. K., Johnson, M., McCoy, T. P., Passmore Griffin, L., & Osborn, C. Y. (2010). Validation of an
organizational communication climate assessment toolkit. American Journal of Medical Quality,
25(6), 436–443. doi:10.1177/1062860610368428
Additional resources can be found in Appendix E and at www.ThinkCulturalHealth.hhs.gov.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 3 64
Bibliography
Cooper, L. A., & Powe, N. R. (2004). Disparities in patient experiences, health care processes, and
outcomes: The role of patient-provider racial, ethnic, and language concordance. Retrieved from
The Commonwealth Fund website:
http://www.commonwealthfund.org/programs/minority/cooper_raceconcordance_753.pdf
Institute of Medicine. (2003). Unequal treatment: Confronting racial and ethnic disparities in health care.
Retrieved from http://www.nap.edu/openbook.php?record_id=10260&page=R1
Institute of Medicine. (2004). In the nation’s compelling interest: Ensuring diversity in the health-care
workforce. Retrieved from http://www.nap.edu/openbook.php?record_id=10885&page=1
The Joint Commission. (2010). Advancing effective communication, cultural competence, and patient-
and family-centered care: A roadmap for hospitals. Retrieved from
http://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf
Passel, J. S., & Cohn, D. (2008). U.S. population projections: 2005-2050. Retrieved from the Pew
Research Center website: http://pewsocialtrends.org/files/2010/10/85.pdf
QSource, Underserved Quality Improvement Organization Support Center. (2005). CLAS Standards
implementation tips. Retrieved from
http://www.qsource.org/uqiosc/CLAS%20Standards%20Strategies%5B7AUG-2005%5D.pdf
Rose, P. R. (2011). Understanding cultural nuances and barriers to cultural appreciation. In P. R. Rose
(Ed.), Cultural competency for health administration and public health (pp. 41–56). Sudbury, MA:
Jones & Bartlett Publishers.
Smedley, B. D., & Mittman, I. S. (2011). The diversity benefit: How does diversity among health
professionals address public needs? In R. A. Williams (Ed.), Healthcare disparities at the
crossroads with healthcare reform (pp. 167–193). New York, NY: Springer.
The Sullivan Commission on Diversity in the Healthcare Workforce. (2004). Missing persons: Minorities in
the health professions. Retrieved from http://www.aacn.nche.edu/media-
relations/SullivanReport.pdf
U.S. Department of Commerce, Census Bureau. (2011). Overview of race and Hispanic origin: 2010.
Retrieved from http://www.census.gov/prod/cen2010/briefs/c2010br-02.pdf
U.S. Department of Commerce, Vice President Al Gore’s National Partnership for Reinventing Government
Benchmarking Study. (1999). Best practices in achieving workforce diversity. Retrieved from
http://govinfo.library.unt.edu/npr/library/workforce-diversity.pdf
U.S. Department of Health and Human Services, Health Resources and Services Administration. (2006).
The rationale for diversity in the health professions: A review of the evidence. Retrieved from
http://bhpr.hrsa.gov/healthworkforce/reports/diversityreviewevidence.pdf

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 3 65
U.S. Department of Health and Human Services, Office of Minority Health. (2001). National standards for
culturally and linguistically appropriate services in health care: Final report. Retrieved from
http://minorityhealth.hhs.gov/assets/pdf/checked/finalreport.pdf
Whealin, J. M., & Ruzek, J. (2008). Program evaluation for organizational cultural competence in mental
health practices. Professional Psychology: Research and Practice, 39, 320–328.
Wynia, M. K., Johnson, M., McCoy, T. P., Passmore Griffin, L., & Osborn, C. Y. (2010). Validation of an
organizational communication climate assessment toolkit. American Journal of Medical Quality,
25(6), 436–443. doi:10.1177/1062860610368428
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 4 66
Standard 4: Educate and Train Governance, Leadership, and
Workforce in CLAS
Standard 4
The National CLAS Standards are intended to advance health equity, improve quality, and help eliminate
health care disparities by establishing a blueprint for health and health care organizations to:
Educate and train governance, leadership, and workforce in culturally and linguistically appropriate
policies and practices on an ongoing basis.
Purpose
The purposes of educating and training governance, leadership, and workforce in CLAS are:
o To prepare and support a workforce that demonstrates the attitudes, knowledge, and skills
necessary to work effectively with diverse populations
o To increase the capacity of staff to provide services that are culturally and linguistically
appropriate
o To assess the progress of staff in developing cultural, linguistic, and health literacy competency
o To foster an individual’s right to respect and nondiscrimination by developing and implementing
education and training programs that address the impact of culture on health and health care
Please refer to the glossary in Appendix A for definitions of the key terms used.
Components of the Standard
Educate and train governance, leadership, and workforce in culturally and linguistically
appropriate services
In order for CLAS to be fully implemented, education and training for professionals working in health and
human services must be ongoing. Cultural and linguistic competency concepts — including effective
communication and patient-, family-, and community-based practices — should be incorporated not only
into all formal educational curricula but also into new and existing staff training and curricula.
Ongoing education and staff training ensures that governance, leadership, and the workforce are
equipped with adequate knowledge, tools, and skills to appropriately manage cross-cultural encounters
with individuals (Betancourt, Green, Carrillo, & Ananeh-Firempong, 2003). Consistent integration of

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 4 67
cultural and linguistic competency with existent educational and training curricula reinforces an
organization’s commitment to providing CLAS and may increase buy-in across the organization based on
improving recognition of the role culture and language play in the provision of care and services,
including their roles in service efficiency, effectiveness, satisfaction, and outcomes (Rose, 2011; Wu &
Martinez, 2006).
While cultural and linguistic competency should permeate all education, training, policies, procedures,
and daily operations, opportunities to learn and hone specific CLAS-related knowledge and skills should
also be available. For example, health profession students should learn about culturally specific
information regarding disease incidence and prevalence or the effect of current and historical events on
certain groups’ interactions with the health and health care system (Betancourt et al., 2003). In addition,
training of governance, leadership, and workforce could include review of, and emphasis on, honing
existing communication or other related skills necessary to work effectively in cross-cultural encounters.
The Joint Commission’s
Advancing Effective Communication, Cultural Competence, and Patient- and
Family-Centered Care: A Roadmap for Hospitals
(2010) states that efforts should include all relevant
policies, services, and programs that pertain to care and services.
Education and training should be based on sound educational principles (e.g., adult learning), including
pre- and post-training assessments, and be conducted by appropriately qualified individuals. For
training, a knowledge-based, skill-based, or attitude-based approach should be adopted, based upon
the needs and weaknesses of the organization, with the goal of ensuring the success of the training
(Rose, 2011). Specific topics for training should be based on the responsibilities of each member of the
workforce, leadership, or governance. Some common topics that might be relevant include (but are not
limited to):
o Exploration of one’s own cultural background and the cultural backgrounds of the individuals and
populations served (AMA, 2006)
o The importance of effective communication to health care outcomes (AMA, 2006)
o Elements of effective communication of staff with individuals or groups of different cultures and
different languages, including how to work with interpreters and use available language services
effectively
o Effects of differences between the cultures of staff and individuals on clinical and other workforce
encounters
o Strategies and techniques for the identification and resolution of cross-cultural conflicts between
staff and individuals or groups and a discussion of the organization’s complaint/grievance
procedures (see Standard 14)

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 4 68
o Effects of cultural differences among individuals and staff on access to care, service utilization,
quality of care, health outcomes, and individuals’ satisfaction, including the importance of socio-
economic status, race, ethnicity, disability status, sexual orientation, gender identity and other
factors
o Importance of learning about the care of, and services to, individuals with limited English
proficiency, low health literacy, disabilities or special needs, and diverse religious and spiritual
backgrounds
o Discussion regarding discrimination based on race, ethnicity, sex, national origin, socioeconomic
status, disability status, religion, sexual orientation, gender identity
o Application of laws and provisions that pertain to the delivery of culturally and linguistically
appropriate care and services, including the Affordable Care Act of 2010, Title VI of the Civil
Rights Act of 1964,
HHS’ Guidance to Federal Financial Assistance Recipients Regarding Title VI
Prohibition Against National Origin Discrimination Affecting Limited English Proficient Persons
(HHS OCR, 2003), Executive Order 13166, and state-level legislation (Graves et al., 2007)
o Strategies for collecting race, ethnicity, sex, language, and disability status data in a sensitive
manner
Finally, there are important potential risks in training about culture, which should be recognized and
addressed. First, training must avoid simplistic generalizations that can lead to stereotyping of individuals
from different cultural groups (AMA, 2006). Instead, training should “emphasize sensitivity to variations
within populations as well as among populations, including individual variations in beliefs, expectations
and preferred modes of communication” and “training should help all members of the workforce develop
the knowledge and skills needed to explore these variations during the course of care or service” (AMA,
2006, p53). Second, it is essential for training to be linked to a comprehensive organizational strategy
around CLAS — to be clearly related to organization mission, goals, and objectives. Thus, training must
be accompanied by coordinated initiatives to support data collection, performance improvement, and
accountability. Training without an organization-wide commitment to CLAS may dilute the training’s long-
term ability to cultivate individuals’ commitment to CLAS if the training establishes performance
expectations that are not then supported throughout the organization.
Strategies for Implementation
The following are possible implementation strategies for educating and training governance, leadership,
and workforce on CLAS:
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 4 69
o Engage staff in dialogues about meeting the needs of diverse populations (Wilson-Stronks &
Galvez, 2007).
o Provide ongoing in-service training on ways to meet the unique needs of the population,
including regular in-services on how and when to access language services for individuals with
limited English proficiency (Wilson-Stronks & Galvez, 2007).
o Take advantage of internal and external resources available to educate governance, leadership,
and workforce on cultural beliefs they may encounter (Wilson-Stronks & Galvez, 2007).
o Allocate resources to train current staff in cultural competency or as medical interpreters if they
speak a second language, have completed language assessments, and show an interest in
interpretation (QSource, 2005).
o Incorporate cultural competency and CLAS into staff evaluations (QSource, 2005).
o Provide opportunities for CLAS training that include regular in-services, brown-bag lunch series,
orientation materials for new staff, and annual update meetings (QSource, 2005).
o Encourage staff to volunteer in the community and to learn about community members and other
cultures (QSource, 2005), and work with community leaders and cultural brokers to create
opportunities for such interactions.
o Evaluate education and training (see Standard 10).
o Take advantage of live and Web-based health disparities and cultural competency continuing
education programs for clinicians and practitioners (Like, 2011).
Resources
American Academy of Family Physicians. (2001).
Quality care for diverse populations videos
[Video
series]. Available from
http://www.aafp.org/online/en/home/clinical/publichealth/culturalprof/quality-care-diverse-
populations.html
American Academy on Communication in Healthcare. (n.d.).
Skills based courses
[Course summaries].
Retrieved from http://www.aachonline.org/?page=SkillsBasedCourses
Cross Cultural Health Care Program. (n.d.).
Course information: Bridging the gap
[Online training course
summary]. Retrieved from http://www.xculture.org/BTGclassdesc.php
Graves, D. L., Like, R. C., Kelly, N., & Hohensee, A. (2007). Legislation as intervention: A survey of
cultural competence policy in health care.
Journal of Health Care Law and Policy, 10
(2), 339–361.
Retrieved from http://thecqc.org/uploads/Graves_et_al.pdf

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 4 70
Institute for Healthcare Communication. (2012).
Training.
Retrieved from
http://healthcarecomm.org/training
Exec. Order No. 13,166, 3 C.F.R. 289 (2000).
Ring, J., Nyquist, J., Mitchell, S., Flores, H., & Samaniego, L. (2008).
Curriculum for culturally responsive
health care: The step-by-step guide for cultural competence training.
Oxford, UK: Radcliffe
Publishing.
U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. (n.d.).
Training and continuing education online:
Health literacy for public health professionals (web-
based)
[Online training course summary]. Retrieved from
http://www2a.cdc.gov/tceonline/registration/detailpage.asp?res_id=2074
U.S. Department of Health and Human Services, Health Resources and Services Administration. (n.d.).
Unified health communication 101.
Retrieved from
http://www.hrsa.gov/publichealth/healthliteracy/index.html
U.S. Department of Health and Human Services, Office for Civil Rights. (2003).
Guidance to federal
financial assistance recipients regarding Title VI and the prohibition against national origin
discrimination affecting limited English proficient persons.
Retrieved from
http://www.hhs.gov/ocr/civilrights/resources/laws/revisedlep.html
U.S. Department of Health and Human Services, Office of Minority Health. (2005).
A patient-centered
guide to implementing language access services in healthcare organizations.
Retrieved from
http://minorityhealth.hhs.gov/Assets/pdf/Checked/HC-LSIG.pdf
U.S. Department of Health and Human Services, Office of Minority Health. (n.d.).
A physician’s practical
guide to culturally competent care.
Retrieved from https://cccm.thinkculturalhealth.hhs.gov/
U.S. Department of Health and Human Services, Office of Minority Health. (n.d.).
Cultural competency
curriculum for disaster preparedness and crisis response.
Retrieved from
https://cccdpcr.thinkculturalhealth.hhs.gov/
U.S. Department of Health and Human Services, Office of Minority Health. (n.d.).
Culturally competent
nursing care: A cornerstone of caring.
Retrieved from https://ccnm.thinkculturalhealth.hhs.gov/
Additional resources can be found in Appendix E and at www.ThinkCulturalHealth.hhs.gov.
Bibliography
American Medical Association. (2006). Improving communication, improving care: How health care
organizations can ensure effective, patient-centered communication with people from diverse
populations. Retrieved from http://www.ama-assn.org/resources/doc/ethics/pcc-consensus-
report.pdf

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 4 71
Betancourt, J. R., Green, A. R., Carrillo, J. E., & Ananeh-Firempong, O. (2003). Defining cultural
competence: A practical framework for addressing racial/ethnic disparities in health and health
care. Public Health Reports, 118, 293–302. Retrieved from
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1497553/pdf/12815076.pdf
Graves, D. L., Like, R. C., Kelly, N., & Hohensee, A. (2007). Legislation as intervention: A survey of
cultural competence policy in health care. Journal of Health Care Law and Policy, 10(2), 339–361.
Retrieved from http://thecqc.org/uploads/Graves_et_al.pdf
The Joint Commission. (2010). Advancing effective communication, cultural competence, and patient-
and family-centered care: A roadmap for hospitals. Retrieved from
http://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf
Like, R. C. (2011). Educating clinicians about cultural competence and disparities in health and health
care. Journal of Continuing Education in the Health Professions, 31(3), 196–206.
QSource, Underserved Quality Improvement Organization Support Center. (2005).CLAS Standards
implementation tips. Retrieved from
http://www.qsource.org/uqiosc/CLAS%20Standards%20Strategies%5B7AUG-2005%5D.pdf
Rose, P. R. (2011). Understanding cultural nuances and barriers to cultural appreciation. In P. R. Rose
(Ed.), Cultural competency for health administration and public health (pp. 41–56). Sudbury, MA:
Jones & Bartlett Publishers.
U.S. Department of Health and Human Services, Office for Civil Rights. (2003). Guidance to federal
financial assistance recipients regarding Title VI prohibition against national origin discrimination
affecting limited English proficient persons. Retrieved from
http://www.hhs.gov/ocr/civilrights/resources/laws/revisedlep.html
Wilson-Stronks, A., & Galvez, E. (2007). Hospitals, language, and culture: A snapshot of the nation.
Retrieved from The Joint Commission website:
http://www.jointcommission.org/assets/1/6/hlc_paper.pdf
Wu, E., & Martinez, M. (2006). Taking cultural competency from theory to action (Commonwealth Fund
Publication No. 964). Retrieved from The Commonwealth Fund website:
http://www.commonwealthfund.org/usr_doc/Wu_takingcultcomptheoryaction_964.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 5 72
Standard 5: Offer Communication and Language Assistance
Standard 5
The National CLAS Standards are intended to advance health equity, improve quality, and help eliminate
health care disparities by establishing a blueprint for health and health care organizations to:
Offer language assistance to individuals who have limited English proficiency and/or other communication
needs, at no cost to them, to facilitate timely access to all health care and services.
Purpose
The purposes of offering communication and language assistance are:
o To ensure that individuals with limited English proficiency and/or other communication needs
have equitable access to health services
o To help individuals understand their care and service options and participate in decisions
regarding their health and health care
o To increase individuals’ satisfaction and adherence to care and services
o To improve patient safety and reduce medical error related to miscommunication
o To help organizations comply with requirements such as Title VI of the Civil Rights Act of 1964;
the Americans with Disabilities Act of 1990; and other relevant federal, state, and local
requirements to which they may need to adhere
Please refer to the glossary in Appendix A for definitions of the key terms used.
Components of the Standard
Offer Language Assistance
Language assistance services are mechanisms used to facilitate communication with individuals who do
not speak English, those who have limited English proficiency, and those who are deaf or hard of hearing.
As noted in The Joint Commission’s
Advancing Effective Communication, Cultural Competence, and
Patient- and Family-Centered Care: A Roadmap for Hospitals
, these services can include in-person
interpreters, bilingual staff, or remote interpreting systems such as telephone or video interpreting, as
well the translation of written materials or signage, sign language, or braille materials (The Joint
Commission, 2010). Language assistance services facilitate the effective and accurate exchange of
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 5 73
information between an individual with language and communication needs and his/her provider. By
facilitating conversations regarding prevention, symptoms, diagnosis, treatment, and other issues,
language assistance improves the quality of services and patient safety.
Language assistance services may be required by law for organizations that receive federal funds. In
2000, the President signed Executive Order 13166, which requires all federal agencies, as well as all
recipients of federal financial assistance, to take reasonable steps to ensure meaningful access for limited
English proficient persons to the services and care provided by their agency or organization (Executive
Order no. 13,166, 2000). This legal requirement stems from the national origin nondiscrimination
provisions of Title VI of the Civil Rights Act of 1964 and its implementing regulations (Executive Order no.
13,166, 2000).
Interpretation and translation can be delivered through a variety of means, depending upon the setting
and the services being delivered. The following table compares and contrasts the acts of interpreting and
translating. As with all culturally and linguistically appropriate services, it is important to monitor the
quality and utilization of services.
Table 3: Interpreting and Translating
Question Interpreting Translating
Why
Interpreting overcomes language barriers
to make communication possible.
Translating allows individuals who cannot read
a specific language to obtain access to written
information in their native tongue.
What
Quality interpreting reflects cultural terms,
expressions, and idioms
that have bearing
on the meaning of the content.
Interpreting must capture any
expressions or nuances in meaning to
maintain the impact of the original
message.
Interpreting is an action that, once having
taken place, is done.
Quality translating must reflect cultural terms,
expressions, and idioms that have bearing on
the meaning of the content. A translation must
capture any expression or nuances in meaning
to maintain the impact of the original message.
A translation is a product that is permanent
and can be shared, stored, reviewed, and
revised as often as desired.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 5 74
Question Interpreting Translating
Who
Interpreters commonly work by
themselves as part of a triad with the
patient and provider. Interpreters must
have an advanced level of proficiency in
both languages and must possess
exceptional listening and memory skills
for accuracy and completeness in verbal
expression.
Special language aptitude is required in
both the language of medical terminology
and in health care systems. Traditionally,
interpreters prepare and conduct research
prior to the encounter, using resources
such as dictionaries and consultation with
professionals in a specific field to
complete their work.
A translator usually works as a part of a
translation team that consists of individuals
with advanced levels of proficiency in both
languages and with exceptional research skills
to ensure accuracy in work. Translation teams
include proofreaders and editors (and in some
cases, desktop publishers, and project
managers).
Special language aptitude is required in both
the language of medical terminology and in
health care systems. Translation teams also
rely on dictionaries, consultation with
professionals in a specific field, and other
resources to complete their work.
How
Interpreters work “in the moment” and
are compelled by the mode of
interpreting. Interpreters may consult
dictionaries or utilize other resources, but
the time between each exchange is only a
matter of seconds or minutes.
Interpreters work bidirectionally, going
back and forth between two languages.
The interpreter functions as a conduit,
clarifier, cultural broker, and advocate.
Interpreters must be able to perform each
role appropriately throughout the
encounter.
Interpreters must be sensitive and
considerate of both cultures. The goal is
to have the listener understand the
message as if it were heard directly from
the original speaker.
The National Council for Interpreting in
Health Care has published a Code of
Ethics and Standards of Practice for
interpreters (National Council on
Interpreting in Health Care, 2004, 2005).
Translators work on a different timeframe.
They must read an entire text for
comprehension before starting the translation,
often consulting dictionaries and other
resources for correct grammar and
terminology.
Most translators usually translate into their
native language(s).
Translation is a process that requires analysis,
conversion, proofreading, and editing.
Translators must be sensitive and considerate
of both cultures. Localization is a specialized
form of translation in which a completely
adapted product (translation) takes into
consideration differences in culture as well as
language, whether that product is software, an
Internet site, or a manufactured product. The
goal is to produce a translation that appears to
have been done originally in the target
country.
The American Translators Association has
issued a Code of Ethics and Professional
Practice for translators (American Translators
Association, n.d.).
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 5 75
Question Interpreting Translating
Where
Interpreting takes place at a specific time
and place.
Interpreters work in public (in a hospital
or clinic, for example) or in private (in the
case of telephonic and video interpreters
who work either from a home office or in
a call center).
Interpreters must be present at a specific
location; i.e., onsite at a hospital or clinic,
or at a location that has dedicated
resources for telephonic interpreting or
video remote interpreting.
Translation can take place at any place and
any time —
only the final product is required to
be at a specific place and time.
Translators work in any setting, from the
offices of a large translation department to the
privacy of their homes.
(National Health Law Program, 2010, pp. 3–4)
Individuals who have limited English proficiency and/or other communication needs
Limited English proficiency is a concept referring to a level of English proficiency that is insufficient to
ensure equal access to public services without language assistance with respect to a particular type of
service, benefit, or encounter (HHS OCR, 2004). As discussed in Standard 1, individuals may have
communication needs not related to a language barrier, such as those who are deaf or hard of hearing,
visually impaired, or disabled or those with low health literacy.
The primary recipient of language assistance is often the individual receiving care or services; however,
other individuals — such as family members or caregivers — may be involved in the provision of support
or care to an individual. If family members or caregivers also have limited English proficiency and/or
other communication needs, their linguistic needs should also be met to ensure the best outcomes for the
individual receiving care. It is important to determine whether the individual’s medical decision-maker,
health care proxy, or advocate has limited English proficiency, since these individuals may serve as the
primary decision-makers regarding the care received by minors, aging parents, and/or individuals with
disabilities (National Health Law Program, 2010).
Timely access to all health care and services
While there is no single definition for “timely” that is universally applicable, the HHS Office for Civil Rights
is available to provide guidance and assistance to those seeking to understand timeliness in access to
services. For example, the Office for Civil Rights notes that language assistance should be provided at a
time and place that avoids the effective denial of the service, benefit, or right at issue or the imposition of
an undue burden on, or delay in, important rights, benefits, or services to the limited English proficient
person (HHS OCR, 2004).
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 5 76
Strategies for Implementation
The following are possible implementation strategies for offering communication and language
assistance:
o Ensure that staff is fully aware of, and trained in, the use of language assistance services,
policies, and procedures (see Standard 4) (HHS OMH, 2005).
o Develop processes for identifying the language(s) an individual speaks (e.g., language
identification flash cards or “I speak” cards) and for adding this information to that person’s
health record (QSource, 2005).
o Use qualified and trained interpreters to facilitate communication (Wilson-Stronks & Galvez,
2007), including ensuring the quality of the language skills of self-reported bilingual staff who use
their non-English language skills during patient encounters (Regenstein, Andres, & Wynia, in
press).
o Establish contracts with interpreter services for in-person, over-the-phone, and video remote
interpreting (HHS OMH, 2005).
o Use cultural brokers when an individual’s cultural beliefs impact care communication (Wilson-
Stronks & Galvez, 2007).
o Provide resources onsite to facilitate communication for individuals who experience impairment
due to a changing medical condition or status (e.g., augmentative and alternative communication
resources or auxiliary aids and services) as noted in
Advancing Effective Communication, Cultural
Competence, and Patient- and Family-Centered Care: A Roadmap for Hospitals
(The Joint
Commission, 2010).
Resources
American Medical Association. (2007).
Office guide to communicating with limited English proficient
patients.
Retrieved from http://www.ama-assn.org/ama1/pub/upload/mm/433/lep_booklet.pdf
Andrulis, D. P., & Brach, C. (2007). Integrating literacy, culture, and language to improve health care
quality for diverse populations.
American Journal of Health Behavior, 31,
S122–S133. Retrieved
from http://www.cpehn.org/pdfs/Integrating%20Literace%20Paper%20-%20Andrulis.pdf
California Academy of Family Physicians. (2005).
Addressing language access issues in your practice: A
toolkit for physicians and their staff members.
Retrieved from
http://www.calendow.org/uploadedFiles/language_access_issues.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 5 77
Chen, A. H., Youdelman, M. K., & Brooks, J. (2007). The legal framework for language access in
healthcare settings: Title VI and beyond.
Journal of General Internal Medicine, 22
(Supplement 2),
362–367. doi:10.1007/s11606-007-0366-2
Divi, C., Koss, R. G., Schmaltz, S. P., & Loeb, J. M. (2007). Language proficiency and adverse events in
US hospitals: A pilot study.
International Journal of Quality in Health Care, 19
(2), 60–67.
doi:10.1093/intqhc/mzl069
The Joint Commission. (2010).
Advancing effective communication, cultural competence, and patient-
and family-centered care: A roadmap for hospitals.
Retrieved from
http://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf
Limited English proficiency: A federal interagency website.
(n.d.). Retrieved from http://www.lep.gov
Robert Wood Johnson Foundation. (2008).
Speaking together toolkit.
Retrieved from
http://www.rwjf.org/pr/product.jsp?id=29653
U.S. Department of Health and Human Services, Office of Minority Health. (2005).
A patient-centered
guide to implementing language access services in healthcare organizations.
Retrieved from
http://minorityhealth.hhs.gov/Assets/pdf/Checked/HC-LSIG.pdf
Additional resources can be found in Appendix E and at www.ThinkCulturalHealth.hhs.gov.
Bibliography
American Translators Association. (n.d.).
Code of ethics and professional practice.
Retrieved from
http://www.atanet.org/membership/code_of_ethics_commentary.pdf
Exec. Order No. 13,166, 3 C.F.R. 289 (2000).
The Joint Commission. (2010).
Advancing effective communication, cultural competence, and patient-
and family-centered care: A roadmap for hospitals.
Retrieved from
http://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf
National Council on Interpreting in Health Care. (2004).
A national code of ethics for interpreters in
health care.
Retrieved from http://www.oregon.gov/OHA/oei/intrprtr/docs/NCIHC_NCE.pdf
National Council on Interpreting in Health Care. (2005).
National standards of practice for interpreters in
health care.
Retrieved from
http://mchb.hrsa.gov/training/documents/pdf_library/National_Standards_of_Practice_for_Interpr
eters_in_Health_Care%20(12-05).pdf
National Health Law Program. (2010).
What’s in a word? A guide to understanding interpreting and
translation in health care.
Retrieved from
http://www.healthlaw.org/images/stories/whats_in_a_word_guide.pdf

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 5 78
QSource, Underserved Quality Improvement Organization Support Center. (2005).
CLAS Standards
implementation tips.
Retrieved from
http://www.qsource.org/uqiosc/CLAS%20Standards%20Strategies%5B7AUG-2005%5D.pdf
Regenstein, M., Andres, E., & Wynia, M. K., for the Commission to End Health Care Disparities. (in press).
Safer use of physicians’ second language skills in caring for patients with limited English
proficiency: A report of the Commission to End Health Care Disparities with recommendations for
clinicians, organizations, and policymakers
. Chicago: IL: American Medical Association.
U.S. Department of Health and Human Services, Office for Civil Rights. (2004).
Limited English proficiency
(LEP).
Retrieved from http://www.hhs.gov/ocr/civilrights/resources/specialtopics/lep/index.html
U.S. Department of Health and Human Services, Office of Minority Health. (2005).
A patient-centered
guide to implementing language access services in healthcare organizations.
Retrieved from
http://minorityhealth.hhs.gov/Assets/pdf/Checked/HC-LSIG.pdf
Wilson-Stronks, A., & Galvez, E. (2007).
Hospitals, language, and culture: A snapshot of the nation.
Retrieved from The Joint Commission website:
http://www.jointcommission.org/assets/1/6/hlc_paper.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 6 79
Standard 6: Inform Individuals of the Availability of Language
Assistance
Standard 6
The National CLAS Standards are intended to advance health equity, improve quality, and help eliminate
health care disparities by establishing a blueprint for health and health care organizations to:
Inform all individuals of the availability of language assistance services clearly and in their preferred
language, verbally and in writing.
Purpose
The purposes of informing individuals of the availability of language assistance are:
o To inform individuals with limited English proficiency, in their preferred language, that language
services are readily available at no cost to them
o To facilitate access to language services
o To help organizations comply with requirements such as Title VI of the Civil Rights Act of 1964;
the Americans with Disabilities Act of 1990; and other relevant federal, state, and local
requirements to which they may need to adhere
Please refer to the glossary in Appendix A for definitions of the key terms used.
Components of the Standard
Inform all individuals of the availability of language assistance services
The provision of language assistance services is critical to ensuring quality, safety, satisfaction, and
improved outcomes, and informing individuals that such services are available helps ensure their use.
Organizations should take the appropriate steps to notify individuals of the availability of language
assistance services and that they are available free of cost. Individuals in need of communication and
language assistance may not know such services are available to them upon request. Commonly reported
barriers to services among individuals who are limited English proficient include the lack of availability of
language services or the lack of awareness that such services exist (Barr & Wanat, 2005; Flores, 2006).
Thus, organizations should provide notification of the availability of language assistance services at
various points of contact and by various means.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 6 80
Language assistance services may be required by law for organizations that receive federal funds. In
2000, the President signed Executive Order 13166, which requires all federal agencies, as well as all
recipients of federal financial assistance, to take reasonable steps to ensure meaningful access for limited
English proficient persons to the services and care provided by their agency or organization (Executive
Order no. 13,166, 2000). This legal requirement stems from the national origin nondiscrimination
provisions of Title VI of the Civil Rights Act of 1964 and its implementing regulations (Executive Order no.
13,166, 2000).
Organizations should provide the notification in the individual’s preferred language as determined by a
language identification tool (e.g., “I speak” cards). Staff and providers speaking to individuals, whether in
person or over the phone, should provide notification of the communication and language assistance
available. Notifications should also be provided in print and multimedia materials that are easy to
understand and translated into the languages commonly used by the populations in the service area
(HHS OMH, 2005).
All members of the organization should be fully aware of the communication and language assistance
services available, as well as all related organizational policies and procedures. To achieve this, all
members of the organization should be trained in how to access communication and language assistance
and work with language assistance personnel in order to support requests that come from individuals
seeking health care and services (see Standard 4). Research conducted by the National Health Law
Program identified staff training as essential to ensuring that available language services are
appropriately utilized (Youdelman, Perkins, Brooks, & Reid, 2007), and another study demonstrated that
more effective staff training is associated with significantly higher ratings on patient-reported quality of
care and trust in the organization (Wynia et al., 2010). These trainings may be conducted in person
onsite (as a part of existing training), or they may be a part of online training and information
dissemination (Youdelman et al., 2007).
To ensure that the organization’s methods of providing notice of language assistance to individuals with
limited English proficiency are effective, the organization should monitor, evaluate, and update the
solutions on an ongoing basis. It may be important to consider the following questions:
o What factors are enablers and barriers to notifying individuals about available language
assistance?
o What aspects of the language assistance notification process should be supported, encouraged,
and replicated?
o What aspects of the language assistance notification process should be revised, improved, or
eliminated?
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 6 81
o What are the recommendations for improving language assistance notification?
o Which of the recommendations should take priority in terms of implementation?
Strategies for Implementation
The following are possible implementation strategies for informing individuals of the availability of
language assistance:
The HHS Office of Minority Health’s
A Patient-Centered Guide to Implementing Language Access Services
in Healthcare Organizations
(2005) identified the following strategies to effectively inform individuals of
the availability of language assistance:
o Determine the content and language of notices
o Decide how to communicate or provide notice to individuals
o Decide where to provide notice to individuals about the availability of assistance
In determining the content and languages of the notices, organizations should consider the following:
o Notification should describe what communication and language assistance is available, in what
languages the assistance is available, and to whom they are available. It should clearly state that
communication and language assistance is provided by the organization free of charge to
individuals (HHS OMH, 2005).
o Notification should be easy to understand at a low literacy level (HHS OMH, 2005).
In deciding how to communicate or provide notice to individuals about the availability of language
services, organizations should consider the following:
o
Signage, Materials, and Multimedia:
Organizations should reflect the languages regularly
encountered in the service area in their signs, materials, and multimedia resources (Berger,
2005; HHS OCR, 2003). For those who may not be literate, information can be conveyed orally or
through signage using symbols or pictures (HHS OMH, 2005; Kashiwagi, 2004).
o
Cultural Mediation:
Another method for promoting quality communication is through the
development of a cultural mediation program. A cultural mediator can act as a liaison between
the culture of the organization and the culture of the individual. An additional strategy for
notifying individuals of language services through mediation is by developing a health promotion
program (e.g., community health workers and promotores de salud) that includes bilingual staff

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 6 82
who train community members to share health and resource information with other community
members (HHS OMH, 2005; Youdelman & Perkins, 2005;).
o
Community Outreach:
Providing notification throughout the community is also important for
reaching those who may be unaware of the organization or what services the organization may
provide. In accordance with Standard 13, consider sending notification through local health
departments, community-based organizations, faith-based organizations, schools, or any other
stakeholders who would benefit from having information on health services (HHS OCR, 2003;
HHS OMH, 2005).
o
Initial Point of Contact:
It is recommended that organizations standardize procedures for staff
members who serve as the initial point of contact for individuals, whether that is by telephone or
in person. It may be appropriate to provide staff with a script to ensure that they inform
individuals of the availability of language assistance and to inquire whether they will need to
utilize any of the available services. Multilingual phone trees and voice mail should also be used
to inform individuals of the available language assistance services and how to access them (HHS
OCR, 2003; HHS OMH, 2005).
o
Non-English Media:
Organizations should publicize availability of language assistance services
in local foreign language media, such as ethnic radio, newspapers, and television (HHS OMH,
2005; Youdelman et al., 2007).
In deciding where to provide notice to individuals about the availability of language services,
organizations should consider the following:
o Points of entry or intake, including:
•
Registration desks
•
Front desks
•
Waiting rooms
•
Financial screening rooms, where individuals may need to discuss and resolve billing
issues
•
Pharmacy reception, where individuals may pick up prescriptions
(HHS OMH, 2005; Kashiwagi, 2004;)
o Areas where clinical work is performed, such as triage and medical exam rooms (HHS OMH,
2005).
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 6 83
Resources
American Medical Association. (2007).
Office guide to communicating with limited English proficient
patients.
Retrieved from http://www.ama-assn.org/ama1/pub/upload/mm/433/lep_booklet.pdf
Brach, C., Fraser, I., & Perez, K. (2005). Crossing the language chasm.
Health Affairs, 24
(2), 424–434.
doi:10.1377/hlthaff.24.2.424
Chen, A. (2006). Doctoring across the language divide.
Health Affairs, 25
(3), 808–813.
doi:10.1377/hlthaff.25.3.808
Limited English proficiency: A federal interagency website.
(n.d.). Retrieved from http://www.lep.gov
Meyers, K., Tang, G., & Fernandez, A. (2009). Responding to the language challenge: Kaiser
Permanente’s approach.
The Permanente Journal, 13
(3), 77–83. Retrieved from
http://www.thepermanentejournal.org/files/Summer2009/language_challenge.pdf
National Association of the Deaf.
(2012). Retrieved from http://www.nad.org/
Robert Wood Johnson Foundation. (n.d.).
Shared decision-making when an interpreter is needed: A case
study with Latino men at risk for prostate cancer
(Grant details). Retrieved from
http://www.rwjf.org/grants/grant.jsp?id=63830
U.S. Department of Health and Human Services, Office of Minority Health. (2005).
A patient-centered
guide to implementing language access services in healthcare organizations.
Retrieved from
http://minorityhealth.hhs.gov/Assets/pdf/Checked/HC-LSIG.pdf
Additional resources can be found in Appendix E and at www.ThinkCulturalHealth.hhs.gov.
Bibliography
Barr, D. A., & Wanat, S. F. (2005). Listening to patients: Cultural and linguistic barriers to health care
access.
Family Medicine, 37,
199–204. Retrieved from
http://www.stfm.org/fmhub/fm2005/March/Donald199.pdf
Berger, C. (2005).
Universal symbols in health care workbook.
Retrieved from Hablamos Juntos website:
http://www.hablamosjuntos.org/signage/PDF/Best%20Practices-FINALDec05.pdf
Exec. Order No. 13,166, 3 C.F.R. 289 (2000).
Flores, G. (2006). Language barriers to health care in the United States.
New England Journal of
Medicine
,
355,
229–231. Retrieved from http://www.nejm.org/doi/full/10.1056/NEJMp058316
Kashiwagi, S. (2004).
A functional manual for providing linguistically competent health care services as
developed by a community health center.
Los Angeles, CA: Asian Pacific Health Care Venture,
Inc.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 6 84
U.S. Department of Health and Human Services, Office for Civil Rights. (2003).
Guidance to federal
financial assistance recipients regarding Title VI and the prohibition against national origin
discrimination affecting limited English proficient persons.
Retrieved from
http://www.hhs.gov/ocr/civilrights/resources/laws/revisedlep.html
U.S. Department of Health and Human Services, Office of Minority Health. (2005).
A patient-centered
guide to implementing language access services in healthcare organizations.
Retrieved from
http://minorityhealth.hhs.gov/Assets/pdf/Checked/HC-LSIG.pdf
Wynia, M. K., Johnson, M., McCoy, T. P., Passmore Griffin, L., & Osborn, C. Y. (2010). Validation of an
organizational communication climate assessment toolkit.
American Journal of Medical Quality,
25
(6), 436–443. doi:10.1177/1062860610368428
Youdelman, M., & Perkins, J. (2005).
Providing language services in small health care provider settings:
Examples from the field
(Commonwealth Fund Publication No. 810). Retrieved from The
Commonwealth Fund website:
http://www.commonwealthfund.org/usr_doc/810_Youdelman_providing_language_services.pdf
Youdelman, M., Perkins, J., Brooks, J. D., & Reid, D. (2007).
Providing language services in state and
local health-related benefits offices: Examples from the field
(Commonwealth Fund Publication
No. 995). Retrieved from The Commonwealth Fund website:
http://www.commonwealthfund.org/~/media/Files/Publications/Fund%20Report/2007/Jan/Provid
ing%20Language%20Services%20in%20State%20and%20Local%20Health%20Related%20Bene
fits%20Offices%20%20Examples%20From%20the%20Fi/Youdelman_providinglanguagesvcsstat
elocalbenefitsoffices_995%20pdf.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 7 85
Standard 7: Ensure the Competence of Individuals Providing
Language Assistance
Standard 7
The National CLAS Standards are intended to advance health equity, improve quality, and help eliminate
health care disparities by establishing a blueprint for health and health care organizations to:
Ensure the competence of individuals providing language assistance, recognizing that the use of
untrained individuals and/or minors as interpreters should be avoided.
Purpose
The purposes of ensuring the competence of individuals providing language assistance are:
o To provide accurate and effective communication between individuals and providers
o To reduce misunderstanding, dissatisfaction, omission of vital information, misdiagnoses,
inappropriate treatment, and patient safety issues due to reliance on staff or individuals that lack
interpreter training
o To empower individuals to negotiate and advocate, on their own behalf, for important services
via effective and accurate communication with health and health care staff
o To help organizations comply with requirements such as Title VI of the Civil Rights Act of 1964;
the Americans with Disabilities Act of 1990; and other relevant federal, state, and local
requirements to which they may need to adhere
Please refer to the glossary in Appendix A for definitions of the key terms used.
Components of the Standard
Ensure the competence of individuals providing language assistance
Before one can be considered qualified to interpret, translate, or provide other communication assistance,
he/she must be assessed to determine his/her competence. Language ability alone does not qualify an
individual to provide language assistance. Leading organizations in the field of language assistance, as
reported by the National Health Law Program (2010), have identified the requisite skills and qualifications
of interpreters as follows:
o Active listening skills

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 7 86
o Message conversion skills
o Clear and understandable speech delivery
o Familiarity with regionalisms and slang in both languages
o Ability to identify differences in meaning due to dialects or regionalisms to ensure effective and
accurate message conversion
o Ability to communicate in all registers and at varying levels of formality
o Understanding of colloquialisms and idiomatic expressions in all working languages
o Working knowledge of anatomy and physiology
o Extensive knowledge of the vocabulary and terminology related to diagnosis, prevention,
treatment, and management of illness and disease
o Understanding of key concepts in health care, such as confidentiality, informed consent, and
patients’ rights
o Command of the vocabulary related to the provision of health care in both languages
A similar list of requisite skills and qualifications has also been compiled by the National Health Law
Program (2010) for translators and is as follows:
o Intimate knowledge of their own native language
o Ability to write in the idiomatic and natural patterns of their native language
o Knowledge of the variety of fields in the health care system and of medical terminology; a basic
knowledge of diseases, procedures, and medications; and knowledge of how the health care
system, as a whole, functions
o Knowledge of their professional limits — especially, before agreeing to translate a document,
being confident that they are qualified to translate it and can make an accurate assessment of
the time it will take to complete the translation
o Good research skills and access to appropriate reference materials
o Expertise in various forms of written communication, from handwritten notes to digital
o Ability to translate medicolegal documents, such as informed consent forms and provisions of the
Health Insurance Portability and Accountability Act

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 7 87
o Regular reading of professional literature in health care fields to maintain currency of information
o Continuous honing of translation skills through professional development courses or training
Use of untrained individuals and/or minors as interpreters should be avoided
Using ad hoc interpreters or untrained individuals and/or minors as interpreters may appear to be a
convenient or reasonable option for the individual and provider alike. For service providers, using an ad
hoc interpreter may appear to be advantageous because there may be little or no upfront financial cost
associated with using untrained individuals and/or minors, and there may be little to no interruption in
service delivery, since the untrained individual is likely readily available. However, the use of unqualified
interpreters can have dire consequences. Grave errors have occurred when untrained individuals have
been used as interpreters, including misdiagnoses and significant medical errors (Flores, 2005; Flores et
al., 2003), which may place the individual at increased risk of significant injury or death. In one notable
case, a first responder misinterpreted a single Spanish word, “intoxicado,” to mean "intoxicated" rather
than its intended meaning of "feeling sick to the stomach." This led to a delay in diagnosis, which
resulted in a potentially preventable case of quadriplegia, and ultimately, a significant malpractice
settlement (Flores, 2006).
Untrained family, friends, minors, and staff often do not possess the necessary skills to provide
meaningful language services. Moreover, given their relationship to the patient, the use of friends, family
members, and minors may compromise the autonomy and confidentiality of the communication (AMA,
2006; Diamond & Jacobs, 2010). There are numerous benefits to the utilization of trained interpreters.
For example, research conducted in an emergency department found that the use of trained interpreters
resulted in reduced return rates to the emergency department, increased clinic utilization, and lower 30-
day discharges, with no concurrent increase in length of stay or cost of visit (Bernstein et al., 2002).
The primary role of the interpreter is to act as the conduit of information between the provider and the
recipient of care or services. Family and friends should be present as a means of support and shared
decision-making if the individual so chooses. However, a loved one should not assume the additional
burden and risk of interpretation errors. Children, especially minor children, may not have the cognitive or
emotional maturity to function in the role of interpreter (Wilson-Stronks & Galvez, 2007). In addition, the
use of children as interpreters has been found not only to place unnecessary tension in the parent-child
relationship but also to place stress and emotional strain on the child (Flores, 2005, 2006; Jacobs, Kroll,
Green, & David, 1995; Schenker, Lo, Ettinger, & Fernandez, 2008). Parents or caregivers may not want
to share sensitive information with their children, and, therefore, health professionals may not be able to
gather an accurate history. It can also be quite distressing for a friend, family member, or child to have
to deliver poor prognostic information to the individual.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 7 88
The use of clinical and nonclinical staff who speak a non-English language but who are untrained in
medical interpretation can pose potential safety risks (Regenstein et al., in press). Research has shown
that when clinicians speak a non-English language, or when untrained bilingual staff is available, an
important set of potential barriers can arise and hinder the effective and appropriate use of trained
interpreters (Maul, Regenstein, Andres, Wright, & Wynia, 2012).
Strategies for Implementation
Depending upon an organization’s size, scope, and mission, its language assistance strategies will differ.
Organizations may opt to provide interpretation services through in-person interpreters and bilingual staff
and providers or through technological or electronic means, including telephonic or video remote
interpreting. Translation may be conducted primarily internally or may be contracted to external
organizations.
The following are possible implementation strategies for ensuring the competence of individuals providing
language assistance:
o Assess the individual’s language ability. There exist many options for testing an individual’s ability
to communicate in a foreign language. The following table summarizes two of the leading
language proficiency scales, the American Council on the Teaching of Foreign Languages scale
(ACTFL) and the Interagency Language Roundtable (ILR) scale (LinguaLinks Library, 1999):
ILR Scale ACTFL Scale Definition
5 Native Able to speak like an educated native speaker
4+
4
Distinguished Able to speak with a great deal of
fluency, grammatical
accuracy, precision of vocabulary and idiomaticity
3+
3
Superior
Able to speak the language with sufficient structural accuracy
and vocabulary to participate effectively in most formal and
informal conversations
2+ Advanced Plus Able
to satisfy most work requirements and show some ability to
communicate on concrete topics
2 Advanced Able to satisfy routine social demands and limited work
requirements
1+ Intermediate - High Able to satisfy most survival needs and limited social demands
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 7 89
ILR Scale ACTFL Scale Definition
1 Intermediate – Mid
Intermediate - Low
Able to satisfy some survival needs and some limited social
demands
Able to satisfy basic survival needs and minimum courtesy
requirements
0+ Novice - High Able to satisfy immediate needs with learned utterances
0 Novice - Mid
Novice - Low
0
Able to operate in only a very limited capacity
Unable to function in the spoken language
No ability whatsoever in the language
o Assess the individual’s ability to provide language assistance. The American Translators
Association upholds standards of practice for translation services (n.d.). Similarly, the National
Council on Interpreting in Health Care has issued standards of practice that define expectations
of performance and outcomes for health care interpreters (2005). In addition, the Certification
Commission for Healthcare Interpreters and the National Board for Certification of Medical
Interpreters provide national certification for interpreters.
The standards of practice identified by these professional organizations may offer promising
practices in the provision of linguistically appropriate services. Keeping these standards at the
core of hiring, training, and evaluating individuals will help ensure their competence in providing
language assistance.
o Employ a “multifaceted model” of language assistance. Organizations may provide language
assistance according to a variety of models, including bilingual staff or dedicated language
assistance (e.g., a contract interpreter or video remote interpreting). A combination of models, or
a multifaceted model, offers the organization a “comprehensive and flexible system [for]
facilitating communication” (National Council on Interpreting in Health Care, 2002, p. 4). Under a
multifaceted model, for example, telephonic interpreting will supplement the language assistance
provided by bilingual staff to ensure that at all times, language assistance is being provided by
competent individuals.
Resources
California Healthcare Interpreting Association.
(n.d.). Retrieved from http://chiaonline.org/

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 7 90
Certification Commission for Healthcare Interpreters.
(n.d.). Retrieved from
http://www.healthcareinterpretercertification.org/
Commonwealth of Massachusetts Executive Office of Health and Human Services, Massachusetts
Department of Public Health. (2004).
Best practice recommendations for hospital-based
interpreter services.
Retrieved from
http://www.hablamosjuntos.org/pdf_files/Best_Practice_Recommendations_Feb2004.pdf
Hablamos Juntos. (2008).
Language testing options 2008.
Retrieved from
http://www.imiaweb.org/uploads/pages/218.pdf
International Medical Interpreters Association. (1995).
Medical interpreting standards of practice.
Retrieved from http://www.hablamosjuntos.org/resources/pdf/IMIA_Standards_Of_Practice.pdf
Limited English proficiency: A federal interagency website.
(n.d.). Retrieved from http://www.lep.gov
National Board of Certification for Medical Interpreters.
(2012). Retrieved from
http://www.certifiedmedicalinterpreters.org/
National Council on Interpreting in Health Care. (2001).
Guide to initial assessment of interpreter
qualifications.
Retrieved from
http://data.memberclicks.com/site/ncihc/NCIHC%20Working%20Paper%20Guide%20to%20Initi
al%20Assessment%20of%20Interpreter%20Qualifications.pdf
Registry of Interpreters for the Deaf. (2012).
Standard practice papers.
Retrieved from
http://www.rid.org/interpreting/Standard%20Practice%20Papers/index.cfm
Robert Wood Johnson Foundation. (2008).
Kaiser Permanente’s health care interpreter certificate
program.
Retrieved from http://www.rwjf.org/pr/product.jsp?id=34036
Robert Wood Johnson Foundation. (2008).
Kaiser Permanente’s qualified bilingual staff model.
Retrieved
from http://www.rwjf.org/pr/product.jsp?id=34030
Trott, J., West, C., Shah, P., & Regenstein, M. (2008).
Building a high-quality language services program
toolkit.
Retrieved from http://www.lawhelp.org/documents/391611Building%20a%20High-
Quality%20Language%20Services%20Program%20Toolkit.pdf
Additional resources can be found in Appendix E and at www.ThinkCulturalHealth.hhs.gov.
Bibliography
American Medical Association. (2006). Improving communication, improving care: How health care
organizations can ensure effective, patient-centered communication with people from diverse
populations. Retrieved from http://www.ama-assn.org/resources/doc/ethics/pcc-consensus-
report.pdf

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 7 91
American Translators Association. (n.d.). Code of ethics and professional practice. Retrieved from
http://www.atanet.org/membership/code_of_ethics_commentary.pdf
Bernstein, J., Bernstein, E., Dave, A., Hardt, E., James, T., Linden, J., Mitchell, P., Oishi, T., & Safi, C.
(2002). Trained medical interpreters in the emergency department: effects on services,
subsequent charges, and follow-up. Journal of Immigrant Health, 4(4), 171-176.
Diamond, L. C., & Jacobs, E. A. (2010). Let’s not contribute to disparities: The best methods for teaching
clinicians how to overcome language barriers to health care. Journal of General Internal
Medicine, 25(Supplement 2), S189–S193. Retrieved from
http://www.springerlink.com/content/00h67538730pl426/fulltext.pdf
Flores, G. (2005). The impact of medical interpreter services on the quality of health care: A systematic
review. Medical Care Research and Review, 62, 255–299.
Flores, G. (2006). Cases from AHRQ WebM&M: Language barriers are more than an inconvenience.
Patient errors range from simple miscommunication to life-threatening. Retrieved from
http://www.medscape.com/viewarticle/534045
Flores, G. (2006). Language barriers to health care in the United States. New England Journal of
Medicine, 355, 229–231. Retrieved from http://www.nejm.org/doi/full/10.1056/NEJMp058316
Flores, G., Laws, M. B., Mayo, S. J., Zuckerman, B., Abreu, M., Medina, L., & Hardt, E. J. (2003). Errors in
medical interpretation and their potential clinical consequences in pediatric encounters.
Pediatrics, 111, 6–14.
Jacobs, B., Kroll, L., Green, J., & David, T. J. (1995). The hazards of using a child as an interpreter.
Journal of the Royal Society of Medicine, 88, 474P–475P. Retrieved from
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1295307/pdf/jrsocmed00067-0056.pdf
LinguaLinks Library. (1999). Correspondence of proficiency scales. Retrieved from
http://www.sil.org/lingualinks/LANGUAGELEARNING/MangngYrLnggLrnngPrgrm/Correspondence
OfProficiencySca.htm
Maul, L., Regenstein, M., Andres, E., Wright, R., & Wynia, M. K. (2012). Using a risk assessment
approach to determine which factors influence whether partially bilingual physicians rely on their
non-English language skills or call an interpreter? The Joint Commission Journal on Quality and
Patient Safety, 38 (7), 328-336.
National Council on Interpreting in Health Care. (2002). Models for the provision of language access in
health care settings. Retrieved from
http://data.memberclicks.com/site/ncihc/NCIHC%20Working%20Paper%20-
%20Models%20for%20Provision%20of%20Language%20Access.pdf
National Council on Interpreting in Health Care. (2005). National standards of practice for interpreters in
health care. Retrieved from

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 7 92
http://mchb.hrsa.gov/training/documents/pdf_library/National_Standards_of_Practice_for_Interpr
eters_in_Health_Care%20(12-05).pdf
National Health Law Program. (2010). What’s in a word? A guide to understanding interpreting and
translation in health care. Retrieved from
http://www.healthlaw.org/images/stories/Whats_in_a_Word_Guide.pdf
Regenstein, M., Andres, E., & Wynia, M. K., for the Commission to End Health Care Disparities. (in press).
Safer use of physicians’ second language skills in caring for patients with limited English
proficiency: A report of the Commission to End Health Care Disparities with recommendations for
clinicians, organizations, and policymakers. Chicago, IL: American Medical Association.
Schenker, Y., Lo, B., Ettinger, K. M., & Fernandez, A. (2008). Navigating language barriers under difficult
circumstances. Annals of Internal Medicine, 149, 264–269.
Wilson-Stronks, A., & Galvez, E. (2007). Hospitals, language, and culture: A snapshot of the nation.
Retrieved from The Joint Commission website:
http://www.jointcommission.org/assets/1/6/hlc_paper.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 8 93
Standard 8: Provide Easy-to-Understand Materials and Signage
Standard 8
The National CLAS Standards are intended to advance health equity, improve quality, and help eliminate
health care disparities by establishing a blueprint for health and health care organizations to:
Provide easy-to-understand print and multimedia materials and signage in the languages commonly used
by the populations in the service area.
Purpose
The purposes of providing easy-to-understand materials and signage are:
o To ensure that readers of other languages and individuals with various health literacy levels are
able to access care and services
o To provide access to health-related information and facilitate comprehension of, and adherence
to, instructions and health plan requirements
o To enable all individuals to make informed decisions regarding their health and their care and
services options
o To offer an effective way to communicate with large numbers of people and supplement
information provided orally by staff members
o To help organizations comply with requirements such as Title VI of the Civil Rights Act of 1964;
the Americans with Disabilities Act of 1990; and other relevant federal, state, and local
requirements to which they may need to adhere
Please refer to the glossary in Appendix A for definitions of the key terms used.
Components of the Standard
Provide easy-to-understand print and multimedia materials and signage
Print and multimedia materials offer an effective way of communicating with large numbers of people,
supplementing information provided by clinicians, service providers, and other staff, and reinforcing key
messages from a health care or service encounter. Therefore, ensuring that an individual can read,
comprehend, and act upon written materials is essential.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 8 94
Unfortunately, many health materials are written at a level too high for the average consumer to
understand (Rudd, Moeykens, & Colton, 2000). The challenge to understand health materials is even
greater for the one-third of adults with limited health literacy (HHS ODPHP, 2010). Minority populations
are disproportionately represented among those with basic or below basic health literacy skills (Kutner et
al., 2006), and the failure to address health literacy may exacerbate disparities (Koh et al., 2012). Health
literate organizations design and distribute print, audiovisual, and social media content that is easy to
understand and act on (Brach et al., 2012). Such materials use appropriate graphics, employ user-
friendly design, focus on actionable information, and refrain from using jargon. Processes should be
established to develop and select materials appropriate for the population served. The National Action
Plan to Improve Health Literacy lays out strategies for developing and disseminating health and safety
information that is accurate, accessible, and actionable (HHS ODPHP, 2010). Health materials should be
used effectively as part of an educational strategy rather than becoming a substitute for spoken
instruction (AHRQ, 2010). Similarly, clear signage does not obviate the need for other navigational
assistance.
It is also important to translate materials that are essential to individuals’ accessing and making educated
decisions about health care, including materials on the internet. Examples of relevant materials include:
o
Administrative and legal documents
— materials requiring informed consent, obligation, or
acknowledgment of certain legal or financial rights and responsibilities; waivers of rights; living
wills and advance directives; emergency room release and discharge forms; marketing materials;
documents establishing and maintaining eligibility for services; explanations of benefit coverage
packages; evidence of coverage cards; and notices of noncoverage
o
Clinical information
— prevention and treatment instructions, including how to prevent
transmission of a communicable disease; what to do before, during, and after a procedure or
treatment (e.g., surgery, chemotherapy); how to take medicine; and how to perform routine self-
care or self-monitoring
o
Education, health prevention and promotion, and outreach materials
— brochures, fact
sheets, pamphlets, promotional flyers and posters, health advisories, and other materials that
support treatment programs (e.g., for chronic disease or mental health) and prevention activities
(e.g., cancer or high blood pressure screenings)
Multilingual signage in the languages of the populations in the service area should provide notices of
rights, the availability of conflict and grievance resolution processes, and directions to facility services. In
addition, wayfinding signage should identify or label the location of specific services.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 8 95
Languages commonly used by the populations in the service area
Easy-to-understand print and multimedia materials and signage should be provided in the languages
commonly used by populations in the service area. The HHS Office for Civil Rights offers guidance for
organizations that receive federal funds to identify the language assistance services that need to be
provided. This guidance will help health and health care organizations determine which documents and
languages are to be addressed. The HHS Office for Civil Rights’ individualized assessment strategy
balances four factors (HHS OCR, 2003):
1. The number or proportion of limited English proficient persons eligible to be served or likely to be
encountered by the program or grantee
2. The frequency with which individuals with limited English proficiency come into contact with the
program
3. The nature and importance of the program, activity, or service provided by the recipient to its
beneficiaries
4. The resources available to the grantee/recipient and the costs of interpretation/translation
services. There is no one-size-fits-all solution for Title VI compliance with respect to limited
English proficient persons, and what constitute reasonable steps for large providers may not be
reasonable where small providers are concerned.
According to guidance from the HHS Office for Civil Rights, organizations that receive federal funds may
be required to take reasonable steps to ensure meaningful access to their programs and activities by
limited English proficient persons. What constitutes meaningful access is made on a case-by-case basis,
and therefore all organizations should determine their level of responsibility by conducting the four-factor
analysis outlined above and developing a language assistance plan (HHS OCR, 2003).
Strategies for Implementation
The following are possible implementation strategies for providing easy-to-understand materials and
signage:
o Issue plain language guidance and create documents that demonstrate best practices in clear
communication and information design (HHS ODPHP, 2010).
o Create forms that are easy to fill out, and offer assistance in completing forms (AHRQ, 2010).
o Consult local librarians to help build an appropriate collection of health materials (HHS ODPHP,
2010).
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 8 96
o Train staff to develop and identify easy-to-understand materials, and establish processes for
periodically re-evaluating and updating materials (AHRQ, 2010).
o Formalize processes for translating materials into languages other than English and for evaluating
the quality of these translations (Wilson-Stronks & Galvez, 2007).
o Develop materials in alternative formats for individuals with communication needs, including
those with sensory, developmental, and/or cognitive impairments as noted in
Advancing Effective
Communication, Cultural Competence, and Patient- and Family-Centered Care: A Roadmap for
Hospitals
(The Joint Commission, 2010).
o Test materials with target audiences. For example, focus group discussions with members of the
target population can identify content in the material that might be embarrassing or offensive,
suggest cultural practices that provide more appropriate examples, and assess whether graphics
reflect the diversity of the target community. Organizations should consider providing financial
compensation or in-kind services to community members who help translate and review materials
(HHS OMH, 2001).
Resources
Centers for Medicare & Medicaid Services. (2011).
The toolkit for making written material clear and
effective: Overview.
Retrieved from https://www.cms.gov/WrittenMaterialsToolkit/
Downing, B., & Bogoslaw, L. (2003).
Translation as a strategy for effective communication with patients
and clients: A how-to guide.
Retrieved from Hablamos Juntos website:
http://www.hablamosjuntos.org/pdf_files/BruceDowningHow-To_Guide_FINAL.pdf
Harvard School of Public Health. (2010).
Health literacy studies: Assessing and developing health
materials.
Retrieved from http://www.hsph.harvard.edu/healthliteracy/practice/innovative-
actions/index.html
Health Literacy Innovations. (2008).
The health literacy & plain language resource guide.
Retrieved from
http://www.healthliteracyinnovations.com/information/RGdownload
Limited English proficiency: A federal interagency website.
(n.d.). Retrieved from http://www.lep.gov
National Council on Interpreting in Health Care. (2010).
Sight translation and written translation:
Guidelines for healthcare interpreters.
Retrieved from
http://data.memberclicks.com/site/ncihc/Translation%20Guidelines%20for%20Interpreters%20R
EVISED%2031710.pdf
National Health Law Program. (2010).
What’s in a word? A guide to understanding interpreting and
translation in health care.
Retrieved from
http://www.healthlaw.org/images/stories/whats_in_a_word_guide.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 8 97
Osborne, H. (2001, November).
In other words…Can they understand? Testing patient education
materials with intended readers.
Retrieved from
http://www.healthliteracy.com/article.asp?PageID=3811 (Reprinted from the
Boston Globe On
Call
magazine)
Pierce, L. (2010). How to choose and develop written educational materials.
Rehabilitation Nursing,
35
(3), 99–105. Retrieved from http://www.rehabnurse.org/pdf/rnj320.pdf
Plain Language Association International.
(2011). Retrieved from http://www.plainlanguagenetwork.org/
Txabarriaga, R. (2009).
IMIA guide on medical translation.
Retrieved from International Medical
Interpreters Association website: http://www.imiaweb.org/uploads/pages/438.pdf
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2010).
Health literacy universal precautions toolkit
(AHRQ Publication No. 10-0046-EF). Retrieved from
http://www.ahrq.gov/qual/literacy/
Additional resources can be found in Appendix E and at www.ThinkCulturalHealth.hhs.gov.
Bibliography
American Medical Association. (2006). Improving communication, improving care: How health care
organizations can ensure effective, patient-centered communication with people from diverse
populations. Retrieved from http://www.ama-assn.org/resources/doc/ethics/pcc-consensus-
report.pdf
Brach, C., Dreyer, D., Schyve, P., Hernandez, L. M., Baur, C., Lemerise, A. J., & Parker, R. (2012).
Attributes of a health literate organization. Retrieved from:
http://www.iom.edu/~/media/Files/Perspectives-Files/2012/Discussion-
Papers/BPH_HLit_Attributes.pdf
The Joint Commission. (2010). Advancing effective communication, cultural competence, and patient-
and family-centered care: A roadmap for hospitals. Retrieved from
http://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf
Koh, H. K., Berwick, D. M., Clancy, C. M., Baur, C., Brach, C., Harris, L. M., & Zerhusen, E. G. (2012).
New federal policy initiatives to boost health literacy can help the nation move beyond the cycle
of costly ‘crisis care’. Health Affairs, 31(2), 434–443.
Kutner, M., Greenberg, E., Jin, Y., & Paulsen, C. (2006). The health literacy of America’s adults: Results
from the 2003 National Assessment of Adult Literacy (NCES 2006–483). Washington, DC:
National Center for Education Statistics.
Rudd, R., Moeykens, B. A., & Colton, T. C. (2000). Health and literacy: A review of the medical and public
health literature. In J. Comings, B. Gerners, & C. Smith (Eds.), Annual review of adult learning
and literacy (pp. 175-203). New York: Jossey-Bass.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 8 98
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2010).
Health literacy universal precautions toolkit (AHRQ Publication No. 10-0046-EF). Retrieved from
http://www.ahrq.gov/qual/literacy/
U.S. Department of Health and Human Services, Office for Civil Rights. (2003). Guidance to federal
financial assistance recipients regarding Title VI and the prohibition against national origin
discrimination affecting limited English proficient persons. Retrieved from
http://www.hhs.gov/ocr/civilrights/resources/laws/revisedlep.html
U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion.
(2010). National action plan to improve health literacy. Retrieved from
http://www.health.gov/communication/HLActionPlan/pdf/Health_Literacy_Action_Plan.pdf
U.S. Department of Health and Human Services, Office of Minority Health. (2001). National standards for
culturally and linguistically appropriate services in health care: Final report. Retrieved from
http://minorityhealth.hhs.gov/assets/pdf/checked/finalreport.pdf
Wilson-Stronks, A., & Galvez, E. (2007). Hospitals, language, and culture: A snapshot of the nation.
Retrieved from The Joint Commission website:
http://www.jointcommission.org/assets/1/6/hlc_paper.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 9 99
Standard 9: Infuse CLAS Goals, Policies, and Management
Accountability Throughout the Organization’s Planning and
Operations
Standard 9
The National CLAS Standards are intended to advance health equity, improve quality, and help eliminate
health care disparities by establishing a blueprint for health and health care organizations to:
Establish culturally and linguistically appropriate goals, policies, and management accountability, and
infuse them throughout the organization’s planning and operations.
Purpose
The purposes of infusing CLAS throughout the organization’s planning and operations are:
o To make CLAS central to the organization’s service, administrative, and supportive functions
o To integrate CLAS throughout the organization (including the mission) and highlight its
importance through specific goals
o To link CLAS to other organizational activities, including policy, procedures, and decision-making
related to outcomes accountability
Please refer to the glossary in Appendix A for definitions of the key terms used.
Components of the Standard
Establish culturally and linguistically appropriate goals, policies, and management
accountability
Establishing goals, policies, and management accountability that promote CLAS throughout an
organization helps to ensure that an organization is culturally and linguistically competent at every point
of contact and ties CLAS to organizational priorities such as individuals’ experiences, satisfaction, safety,
and outcomes. This also illustrates the relevance of CLAS even in times of budgetary constraints and
limited resources (Wu & Martinez, 2006). In addition, this integrated approach demonstrates to the
community that cultural and linguistic competency is integral to the organization’s mission and vision.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 9 100
Infuse CLAS throughout the organization’s planning and operations
Culturally and linguistically appropriate services should be embedded throughout all levels of the
organization—from the top down and from the bottom up. The entire health or health care organization
affects quality of services and health outcomes of individuals; therefore, the entire organization should
fully integrate CLAS- and health equity–related concepts and ideals. Different departments, policies, and
roles should coordinate with and complement each other to this end.
Health and health care organizations should incorporate CLAS goals, policies, and accountability
procedures at all levels by making them key aspects of the organization’s planning and operations
(Weech-Maldonado, 2002). Organizations are encouraged to embed CLAS as a core element of the
organization’s identity, mission, operating principles, service focus, budget, and quality improvement
activities (AMA, 2006). For example, a health organization might collect and merge individual-level
demographic data and quality improvement measures together to illustrate equitable health care as a
quality improvement goal (Wilson-Stronks & Galvez, 2007).
In addition, organizations should establish a method (or procedure) of accountability for CLAS activities
throughout the organization’s hierarchy, from the front desk to the senior executive level. All members of
the organization should be trained and supported in making their day-to-day responsibilities culturally and
linguistically appropriate and should be evaluated based on criteria relevant to CLAS and their role(s)
within the organization (see Standard 4).
The National Quality Forum includes integration of cultural competency into management systems and
operations as one of its seven primary domains for measuring and reporting cultural competency.
Specifically, the National Quality Forum notes that a focus “on whether cultural competency is integrated
throughout all management and operations activities of the organization is an essential component of
supporting the delivery of culturally competent care” (National Quality Forum, 2009, p. iv).
Strategies for Implementation
The following are possible implementation strategies for infusing CLAS goals, policies, and management
accountability throughout the organization’s planning and operations:
o Engage the support of governance and leadership, and encourage the allocation of resources to
support the development, implementation, and maintenance of culturally and linguistically
appropriate services.
o Encourage governance and leadership to establish education and training requirements relating
to culturally and linguistically appropriate services for all individuals in the organization, including
themselves.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 9 101
o Identify champions within and outside the organization to advocate for CLAS, to emphasize the
business case and rationale for CLAS, and encourage full-scale implementation.
o Hold organizational retreats to identify goals, objectives, and timelines to provide culturally and
linguistically appropriate services.
o Establish accountability mechanisms throughout the organization, including staff evaluations,
individuals’ satisfaction measures, and quality improvement measures (QSource, 2005).
o Utilize the data gathered based on Standards 10, 11, and 12 to guide plan development.
o In accordance with Standard 13, involve the populations in the service area in the
implementation of CLAS through the strategic plan.
Resources
Betancourt, J. R., Weissman, J. S., Kim, M. K., Park, E., & Maina, A. W. (2007).
Resident physicians’
preparedness to provide cross-cultural care: Implications for clinical care and medical education
policy
. Retrieved from The Commonwealth Fund website:
http://www.commonwealthfund.org/usr_doc/1026_Betancourt_resident_MDs_preparedness_prov
ide_cross-cultural_care.pdf
The Joint Commission. (2007).
“What did the doctor say?”: Improving health literacy to protect patient
safety.
Retrieved from
http://www.jointcommission.org/assets/1/18/improving_health_literacy.pdf
Roat, C. (2003).
How to choose and use a language agency: A guide for health and social service
providers who wish to contract with language agencies.
Retrieved from The California
Endowment website:
http://www.calendow.org/uploadedFiles/how_to_choose_use_language_agency.pdf
Weech-Maldonado, R. (2007, June).
Moving towards culturally competent health systems: Organizational
and market factors.
Presented at the AcademyHealth Disparities Interest Group Meeting, Miami,
FL. Retrieved from http://www.academyhealth.org/files/interestgroups/disparities/weech-
maldonador.pdf
Wilson-Stronks, A., & Galvez, E. (2007).
Hospitals, language, and culture: A snapshot of the nation.
Retrieved from The Joint Commission website:
http://www.jointcommission.org/assets/1/6/hlc_paper.pdf
Wu, E., & Martinez, M. (2006).
Taking cultural competency from theory to action
(Commonwealth Fund
Publication No. 964). Retrieved from The Commonwealth Fund website:
http://www.commonwealthfund.org/usr_doc/Wu_takingcultcomptheoryaction_964.pdf
Additional resources can be found in Appendix E and at www.ThinkCulturalHealth.hhs.gov.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 9 102
Bibliography
American Medical Association. (2006). Improving communication, improving care: How health care
organizations can ensure effective, patient-centered communication with people from diverse
populations. Retrieved from http://www.ama-assn.org/resources/doc/ethics/pcc-consensus-
report.pdf
National Quality Forum. (2009). A comprehensive framework and preferred practices for measuring and
reporting cultural competency: A consensus report. Retrieved from
http://www.qualityforum.org/Publications/2009/04/A_Comprehensive_Framework_and_Preferred
_Practices_for_Measuring_and_Reporting_Cultural_Competency.aspx
QSource, Underserved Quality Improvement Organization Support Center. (2005). CLAS Standards
implementation tips. Retrieved from
http://www.qsource.org/uqiosc/CLAS%20Standards%20Strategies%5B7AUG-2005%5D.pdf
Weech-Maldonado, R. (2002). Organizational support standards for culturally and linguistically
appropriate services (CLAS): Core concepts, content knowledge, and core skills. Retrieved from
https://www.thinkculturalhealth.hhs.gov/pdfs/PhysiciansConceptPaper_Weech_Maldanado.pdf
Wilson-Stronks, A., & Galvez, E. (2007). Hospitals, language, and culture: A snapshot of the nation.
Retrieved from The Joint Commission website:
http://www.jointcommission.org/assets/1/6/hlc_paper.pdf
Wu, E., & Martinez, M. (2006). Taking cultural competency from theory to action (Commonwealth Fund
Publication No. 964). Retrieved from The Commonwealth Fund website:
http://www.commonwealthfund.org/usr_doc/Wu_takingcultcomptheoryaction_964.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 10 103
Standard 10: Conduct Organizational Assessments
Standard 10
The National CLAS Standards are intended to advance health equity, improve quality, and help eliminate
health care disparities by establishing a blueprint for health and health care organizations to:
Conduct ongoing assessments of the organization’s CLAS-related activities and integrate CLAS-related
measures into measurement and continuous quality improvement activities.
Purpose
The purposes of conducting organizational assessments are:
o To assess performance and monitor progress in implementing the National CLAS Standards
o To obtain information about the organization and the people it serves, which can be used to
tailor and improve services
o To assess the value of CLAS-related activities relative to the fulfillment of governance, leadership,
and workforce responsibilities
Please refer to the glossary in Appendix A for definitions of the key terms used.
Components of the Standard
Conduct ongoing assessment of the organization’s CLAS-related activities
In general, the continuous quality improvement process for CLAS includes an assessment phase, a
planning phase, an implementation phase, and an evaluation phase (Briefer French et al., 2008). As a key
initial step in the continuous quality improvement process, organizational self-assessment is often used to
examine factors that might enable or impede a service delivery system’s effectiveness and performance.
It is essential for planning, implementing, and evaluating the quality of any kind of service, including
CLAS. To address organizational readiness for providing CLAS, The Joint Commission’s
Advancing
Effective Communication, Cultural Competence, and Patient- and Family-Centered Care: A Roadmap for
Hospitals
(2010) calls on hospitals to “conduct an organization assessment that measures baseline
performance on specific issues to know where improvement might be necessary, detect gaps and areas
of excellence, and tailor improvement interventions.”
Organizational assessments range in intensity from relatively brief self-assessments using input solely
from those in supervisory and/or administrative positions (e.g., organizational checklists), to in-depth

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 10 104
assessments with structured and formal input from stakeholders, patients, consumers, and/or staff. In
addition, they employ data collection methods ranging from informal interviews with senior leaders to
using validated surveys across the organization. Ultimately, they produce outputs ranging from general
and broad guidance to benchmarked and validated scores across multiple domains of performance.
A cultural audit is an assessment strategy used to examine, among other factors, an organization’s
values, symbols, and routines and identify problems that affect the organization’s ability to provide
services (Rice, 2005, 2008). A cultural audit may be used specifically to develop CLAS. With regard to
cultural and linguistic competency, many organizations may remain largely unaware of structural,
procedural, and behavioral factors that create barriers to providing quality services for diverse
populations. A cultural audit and self-assessment may increase awareness within the organization by
facilitating the identification of unique group characteristics that can be used to ensure service access and
treatment and the identification of opportunities for the organization to better market itself to diverse
populations (Andrulis, Delbanco, Avakian, & Shaw-Taylor, 2001). Although many health and health care
organizations are attempting to provide CLAS through targeted programs, research suggests that they
rarely perform optimally across the range of issues associated with CLAS (Wynia et al., 2010). Too often,
these efforts are not linked with other organizational activities that focus on policy and decision-making
related to outcomes accountability. A comprehensive audit, however, can help organizations identify the
existing gaps between CLAS programming and initiatives and widespread organizational policies that can
support, sustain, and ultimately improve such initiatives (Wynia et al., 2010).
Integrate CLAS-related measures into measurement and continuous quality improvement
activities
Integrating measures related to cultural and linguistic competency into existing assessment efforts and
continuous quality improvement programs helps organizations learn whether CLAS delivery processes are
producing the desired results. Without incorporating such measures into assessment, planning,
implementation, and evaluation efforts, organizations will not be able to demonstrate successfully the
effectiveness of CLAS delivery, nor will they be able to identify ways to improve CLAS implementation.
CLAS-related measures in performance improvement and outcomes assessments include but are not
limited to:
o Accessibility of interpreter services
o Effectiveness of cultural and linguistic competency training for providers and nonclinical staff
o Differences in the use of services among diverse populations
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 10 105
o Impact of culturally and linguistically competent service provision on health outcomes and health
status and on individuals’ satisfaction
Strategies for Implementation
The following are possible implementation strategies for conducting organizational assessments:
o Conduct an organizational assessment or a cultural audit using existing cultural and linguistic
competency assessment tools to inventory structural policies, procedures, and practices. These
tools can provide guidance to determine whether the core structures and processes (e.g.,
management, governance, delivery systems, and customer relation functions) necessary for
providing CLAS are in place.
o Use results from assessments to identify assets (e.g., bilingual staff members who could be used
as interpreters, existing relationships with community-based ethnic organizations), weaknesses
(e.g., no translated signage or cultural competency training), and opportunities to improve the
organization’s structural framework and capacity to address cultural and linguistic competence in
care (e.g., revise mission statement, recruit people from diverse cultures into policy and
management positions).
o Following the assessment, prepare adequate plans for developing CLAS (see Standard 9).
Subsequent ongoing assessment helps organizations to monitor their progress in implementing
the enhanced National CLAS Standards and to refine their strategic plans.
The following are implementation strategies for integrating CLAS-related measures into measurement and
continuous quality improvement activities (QSource, 2005):
o Implement ongoing organizational assessment of CLAS-related activities
o Provide individuals with CLAS-oriented feedback forms and include self-addressed, stamped
envelopes to improve receipt of feedback
o Conduct focus groups with individuals to monitor progress and identify barriers to full-scale CLAS
implementation
o Assess the standard of care provided for various chronic conditions to determine whether
services are uniformly provided across cultural groups
o Add CLAS-related questions to staff orientation materials and yearly reviews
o Develop a system of reviewing and incorporating feedback and suggestions received and for
monitoring their effect on CLAS implementation and outcomes
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 10 106
o Identify outcome goals, including metrics, regarding cultural and linguistic competency and
assess at regular intervals
Resources
American Medical Association. (n.d.).
Communication climate assessment toolkit
. Retrieved from
http://www.ama-assn.org/go/ccat
Beach, M. C., Cooper, L. A., Robinson, K. A., Price, E. G., Gary, T. L., Jenckes, M. W., … Powe, N. R.
(2004).
Strategies for improving minority healthcare quality
(AHRQ Publication No. 04-E008-02).
Retrieved from Agency for Healthcare Research and Quality website:
http://archive.ahrq.gov/downloads/pub/evidence/pdf/minqual/minqual.pdf
Campinha-Bacote, J. (2002).
Inventory for assessing the process of cultural competence among
healthcare professionals-Revised (IAPCC-R).
Retrieved from
http://www.transculturalcare.net/iapcc-r.htm
Drucker, P. F. (1998).
The Drucker Foundation self-assessment tool: Participant workbook.
Hoboken, NJ:
Jossey-Bass, Inc.
Hasnain-Wynia, R., & Baker, D. W. (2006). Obtaining data on patient race, ethnicity, and primary
language in health care organizations: Current challenges and proposed solutions.
Health
Services Research, 41,
1501–1518. doi:10.1111/j.1475-6773.2006.00552.x
Johns Hopkins University. (2010).
COA360.
Retrieved from www.COA360.org
National Center for Cultural Competence, Georgetown University Center for Child and Human
Development, Georgetown University Medical Center. (n.d.).
Cultural competence health
practitioner assessment (CCHPA).
Retrieved from
http://nccc.georgetown.edu/features/CCHPA.html
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2008).
Hospital language services: Quality improvement and performance measures. In
Advances in
patient safety: New directions and alternative approaches, Volume 2. Culture and redesign
(AHRQ Publication No. 08-0034-2). Retrieved from http://www.ncbi.nih.gov/books/NBK43719
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2011).
Surveys on patient safety culture
. Retrieved from http://www.ahrq.gov/qual/patientsafetyculture/
Vogt, K. (2006, September). Mystery shopping gaining popularity in health care sector: The rise of
consumer-directed care is one reason why physicians, hospitals and health plans are sending
people incognito to learn how things are working.
American Medical News.
Retrieved from
http://www.ama-assn.org/amednews/2006/09/18/bise0918.htm
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 10 107
Wang, S. (2006, August 8). Health care taps “mystery shoppers”: To improve service, hospitals and
doctors hire spies to pose as patients and report back.
Wall Street Journal.
Retrieved from
http://online.wsj.com/article/SB115499684792929340.html
Additional resources can be found in Appendix E and at www.ThinkCulturalHealth.hhs.gov.
Bibliography
Andrulis, D., Delbanco, T., Avakian, L., & Shaw-Taylor, Y. (2001).
Conducting a cultural competence self-
assessment
. Retrieved from http://erc.msh.org/provider/andrulis.pdf
Briefer French, J., Schiff, D., Han, E., & Weinick, R. (2008).
Multicultural health care: A quality
improvement guide.
Retrieved from National Committee for Quality Assurance website:
http://www.ncqa.org/Portals/0/HEDISQM/CLAS/CLAS_toolkit.pdf
The Joint Commission. (2010). A
dvancing effective communication, cultural competence, and patient-
and family-centered care: A roadmap for hospitals
. Retrieved from
http://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf
QSource, Underserved Quality Improvement Organization Support Center. (2005).
CLAS Standards
implementation tips.
Retrieved from
http://www.qsource.org/uqiosc/CLAS%20Standards%20Strategies%5B7AUG-2005%5D.pdf
Rice, M. F. (2005). Teaching public administration education in the post modern era. In M. F. Rice (Ed.),
Diversity and public administration: Theory, issues, and perspectives
(pp. 87–103). Armonk, NY:
Sharpe.
Rice, M. F. (2008). A primer for developing a public agency service ethos of cultural competency in public
services programming and public services delivery.
Journal of Public Affairs Education, 14,
21–38.
Wynia, M. K., Johnson, M., McCoy, T. P., Passmore Griffin, L., & Osborn, C. Y. (2010). Validation of an
organizational communication climate assessment toolkit.
American Journal of Medical Quality,
25
(6), 436–443. doi:10.1177/1062860610368428
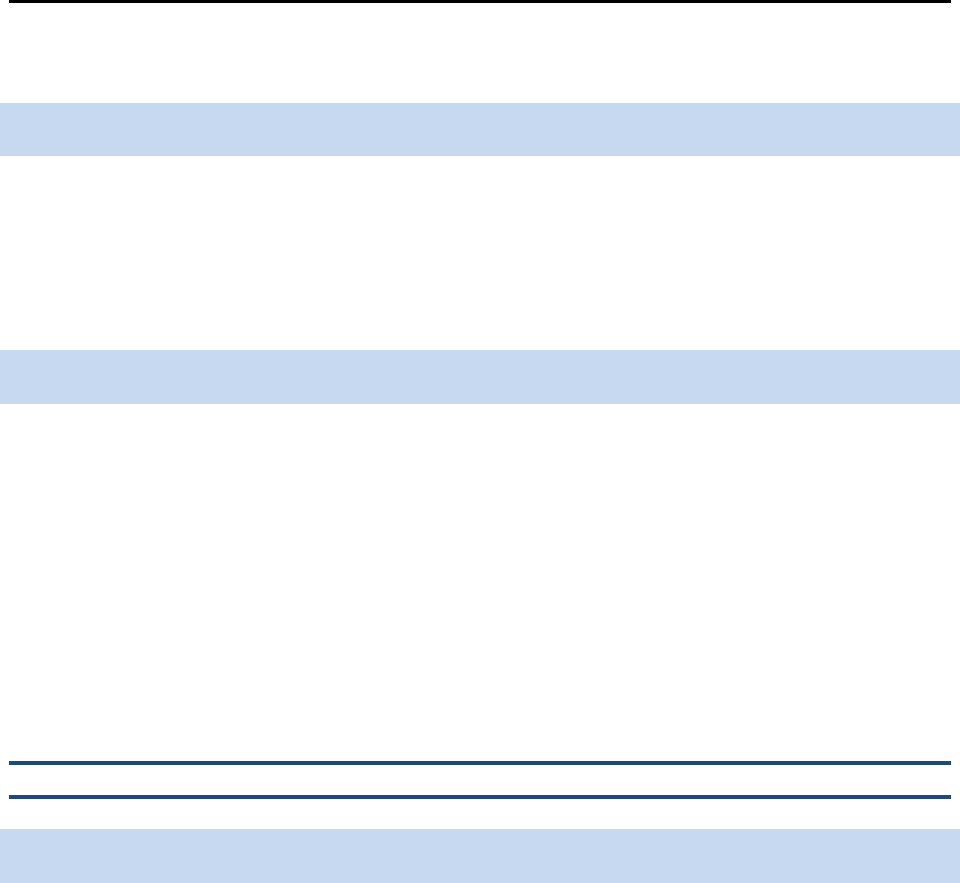
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 11 108
Standard 11: Collect and Maintain Demographic Data
Standard 11
The National CLAS Standards are intended to advance health equity, improve quality, and help eliminate
health care disparities by establishing a blueprint for health and health care organizations to:
Collect and maintain accurate and reliable demographic data to monitor and evaluate the impact of CLAS
on health equity and outcomes and to inform service delivery.
Purpose
The purposes of collecting and maintaining demographic data are:
o To accurately identify population groups within a service area
o To monitor individual needs, access, utilization, quality of care, and outcome patterns
o To ensure equal allocation of organizational resources
o To improve service planning to enhance access and coordination of care
o To assess and improve to what extent health care services are provided equitably
Please refer to the glossary in Appendix A for definitions of the key terms used.
Components of the Standard
Collect and maintain accurate and reliable demographic data
Health and health care organizations should collect key data from individuals using personnel trained in
cultural and linguistic competency. Data collected should include demographic information such as race,
ethnicity, sex, language, and disability status (HHS, 2011ab). When elements of such data are collected
in different ways across different sectors of the health and health care system and by separate
organizations, the data are fragmented and often poorly integrated (IOM, 2009; National Research
Council, 2009).
The availability of demographic data, particularly race and ethnicity, is the first step in being able to
demonstrate the effectiveness of CLAS in the delivery of quality, equitable care and, ultimately, in
reducing disparities (Hasnain-Wynia & Baker, 2006; Nerenz, 2005; HHS, 2011b). Other reasons to collect
data pertaining to CLAS are (Massachusetts Department of Public Health, Office of Health Equity, 2009):

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 11 109
o To meet state and federal reporting requirements, including new requirements being
implemented under health reform
o To establish the foundation for cultural and linguistic competency
o To become more responsive to cultural preferences
o To tailor services to diverse needs
o To use resources more cost effectively
o To become more competitive in the market place
In organizations with multiple points of entry, information collected at one point should be routinely
shared across other service sectors or departments consistent with the confidentiality requirements (see
p119). Ideally, for programs requiring enrollment (e.g., managed care programs), the person responsible
for enrollment would collect these data and then share the information with the provider. In other cases,
health professionals, such as physicians or pharmacists, could collect and record this information at the
first point of contact (Wynia, Ivey, & Hasnain-Wynia, 2010). The information should be included in the
individual’s record and communicated to other departments that might have contact with the individual,
such as billing or member services. The utilization of electronic health records and other health
information technology (HIT) systems could significantly facilitate this sharing of data within and between
organizations (IOM, 2009).
To ensure the accuracy and reliability of the data collected, organizations should facilitate processes that
allow for self-identification and avoid use of observational/visual assessment methods, the latter of which
is considered to be less reliable (Hasnain-Wynia & Baker, 2006; Hasnain-Wynia, Pierce, & Pittman, 2004;
Higgins & Taylor, 2009). If a demographic variable (e.g., race) has more than one category, individuals
should be allowed to indicate all categories that apply. In addition, with the increased adoption of health
information technology, organizations have another way to improve upon the collection and exchange of
reliable data (IOM, 2009).
In October 2011, the U.S. Department of Health and Human Services released implementation guidance
for the collection of race, ethnicity, sex, primary language, and disability status data (HHS, 2011b). The
purpose of the guidance was to promulgate a set of uniform data collection standards for inclusion in
population-health surveys conducted or sponsored by HHS as required by Section 4302 of the Affordable
Care Act.
In addition to the standards below, HHS is developing a national data progression plan on sexual
orientation and gender identity variables.
The Blueprint
will be updated accordingly to reflect the most
current HHS requirements.
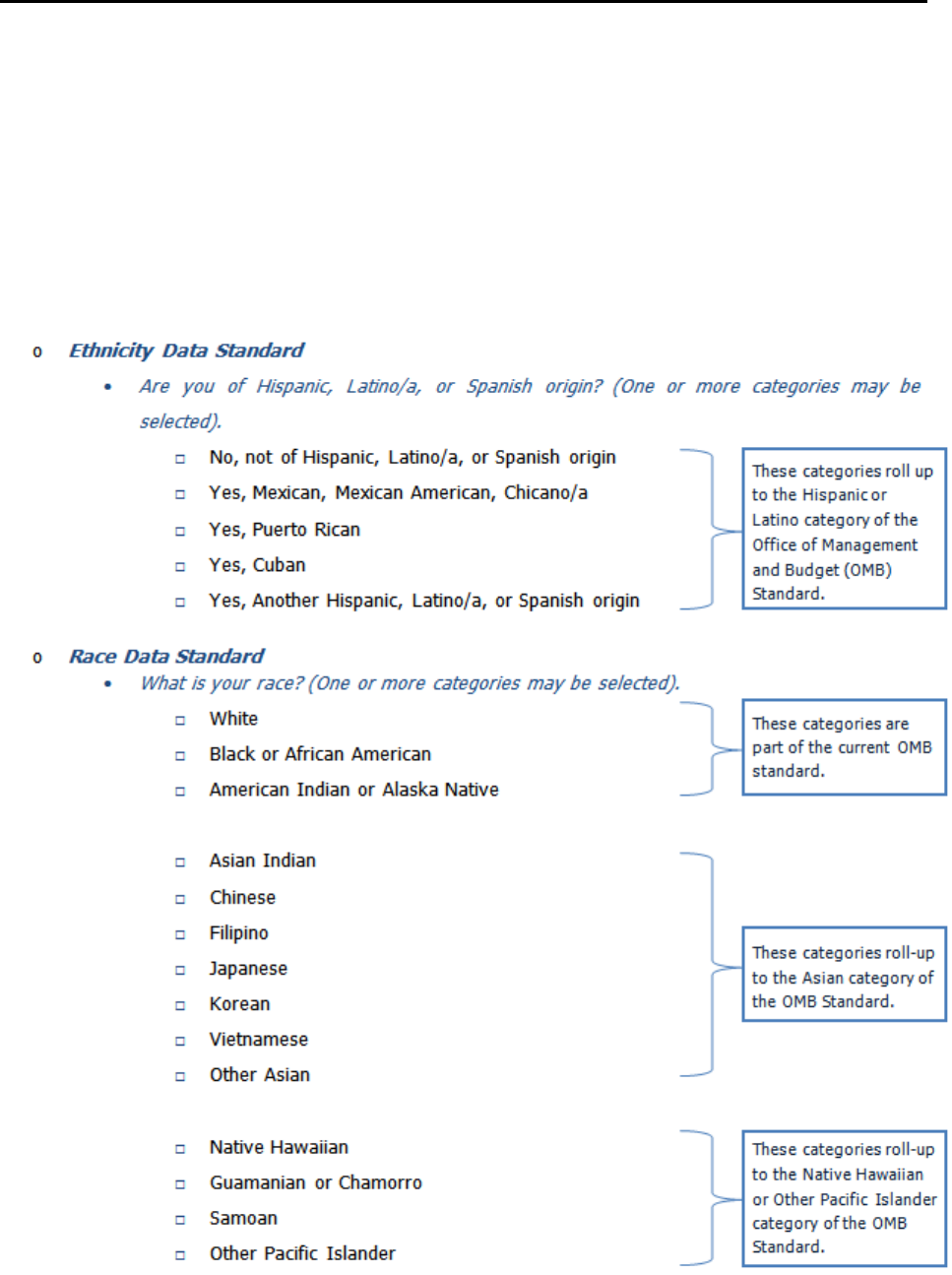
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 11 110
The HHS implementation guidance is clear in its intent that the data collection standards represent the
minimum, not the maximum, requirements. The variables noted in the guidance are not intended to limit
the collection of needed data. Agencies are encouraged to collect additional data as needed, as long as
the minimum standard is included, the data can be aggregated up to the minimum standard (in the case
of race and ethnicity), and the sample size supports those estimates. For the disability data standard,
although survey questions and answer categories included in the standard cannot be changed, additional
disability questions may be included.
HHS Data Collection Standards (HHS, 2011a)

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 11 111
o
Sex Data Standard
•
What is your sex?
□ Male
□ Female
o
Primary Language Data Standard
•
How well do you speak English? (5 years old or older)
□ Very well
□ Well
□ Not well
□ Not at all
Recommended additional questions
•
Do you speak a language other than English at home? (5 years old or older)
□ Yes
□ No
For persons speaking a language other than English (answering yes to the question above):
•
What is this language? (5 years old or older)
□ Spanish
□ Other Language (Identify)
o
Disability Status Data Standard
•
Are you deaf or do you have serious difficulty hearing?
□ Yes
□ No
•
Are you blind or do you have serious difficult seeing, even when wearing glasses?
□ Yes
□ No
•
Because of a physical, mental, or emotional condition, do you have serious difficulty
concentrating, remembering, or making decisions? (5 years old or older)
□ Yes
□ No
•
Do you have serious difficulty walking or climbing stairs? (5 years old or older)
□ Yes
□ No
•
Do you have difficulty dressing or bathing? (5 years old or older)
□ Yes
□ No

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 11 112
•
Because of a physical, mental, or emotional condition, do you have difficulty doing
errands alone, such as visiting a doctor’s office or shopping? (15 years old or older)
□ Yes
□ No
To monitor and evaluate the impact of CLAS on health equity and outcomes and to inform
service delivery
Ultimately, one purpose of collecting and maintaining accurate demographic data is to utilize the data in
organizational monitoring, evaluation, and continuous quality improvement activities (IOM, 2009; Wynia
et al., 2010). In addition, while the assessment of health disparities and inequities is complex and entails
linking demographic data with other types of data (e.g., service data, quality of care data), the availability
of accurate and reliable demographic data is key in documenting such issues and developing strategies to
address them (Bilheimer & Klein, 2010; Hasnain-Wynia & Baker, 2006; IOM, 2009; Lurie & Fremont,
2006).
Organizations may use demographic data to determine basic information about trends in organizational
and health care utilization, such as the total number of visits made to emergency departments based on
race/ethnicity and gender or the total number of individuals requesting language assistance. This
information could then be used to make staffing assignment decisions or determine the need for
additional language assistance resources. When linked with other data, health and health care
organizations can make increased data-informed decisions and improve the quality of care, consistent
with quality improvement activities (Fiscella, 2011). For example, in response to changing state
regulations on the collection of race/ethnicity/language data, several hospitals in Massachusetts began
linking these data with performance and quality measures to identify disparities in health and health care,
develop targeted programs for employees concerning cultural competency, and develop targeted
interventions to engage individuals from specific populations (Jorgensen, Thorlby, Weinick, & Ayanian,
2010).
Current surveys and data collection tools may not encompass all demographic groups in a particular area
or region. For example, although lesbian, gay, bisexual and transgender related data have been collected
on several surveys in the past, there are a number of challenges (HHS, 2012). This can limit the ability to
estimate population size and address health needs. Organizations should sensitively and strategically
utilize, and develop if necessary, survey instruments that will encompass the various demographic groups
in their community. Partnerships, as described in Standard 13, can assist in the identification and
development of such instruments.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 11 113
Confidentiality Issues
In collecting data, organizations will likely encounter issues related to confidentiality. Many individuals
may be hesitant to provide personal information, such as race, ethnicity, and language, due to concerns
about privacy or fear of negative reprisals (IOM, 2009; Robert Wood Johnson Foundation, 2004).
Individuals may believe that they will receive disparate services based on their answers to questions
about race, ethnicity, primary language, gender identity, or sexual orientation in a health or service
encounter. Still others may worry about being asked to pay higher insurance premiums based on race,
ethnicity, or would either say medical condition or pre-existing condition.
Data collection should not be at the detriment of the relationship between the individual and the health
care or service provider, and the individual should not be put at risk to collect such data. Just as
important is the organization’s obligation to inform individuals and, ideally, all groups in the community
about the purpose of collecting such data, the intended uses of the data, and the individual’s right to
withhold the data. Individuals need to be assured that the information is being gathered for legitimate
purposes, and they should be notified as to the circumstances in which their data will be shared (AHRQ,
2011; Lurie & Fremont, 2006). In addition to following ethical principles and standards, health care
organizations should follow the federal regulation concerning the privacy of health information. The
Privacy Rule under the Health Insurance Portability and Accountability Act of 1996 requires health care
organizations and providers to collect, use, and/or disclose individually identifiable data and information
only to the extent necessary to accomplish a specific purpose and to obtain consent for both routine and
nonroutine use and disclosure of health records. The regulation also calls for organizations and providers
to provide a clear, written explanation of how health information can and will be used, kept, and
disclosed (HHS ODPHP, 2000).
To maintain the confidentiality and privacy of potentially identifiable data, there are a number of options
organizations and providers could choose. For example, organizations and providers could de-identify the
data or use codes for data, such as race and ethnicity information, that would not be linked to individuals’
names. These de-identified data could then be analyzed and reported in aggregate to monitor disparities
and measure outcomes. In addition, organizations could clarify the purpose of the data to staff and
specify which staff members may have access to the data. In establishing and enforcing data collection
and access policies and procedures, organizations should also ensure that all staff members with data
access regularly receive training on client record confidentiality (HHS OMH, 2001).
Strategies for Implementation
The following are possible implementation strategies for collecting and maintaining demographic data:
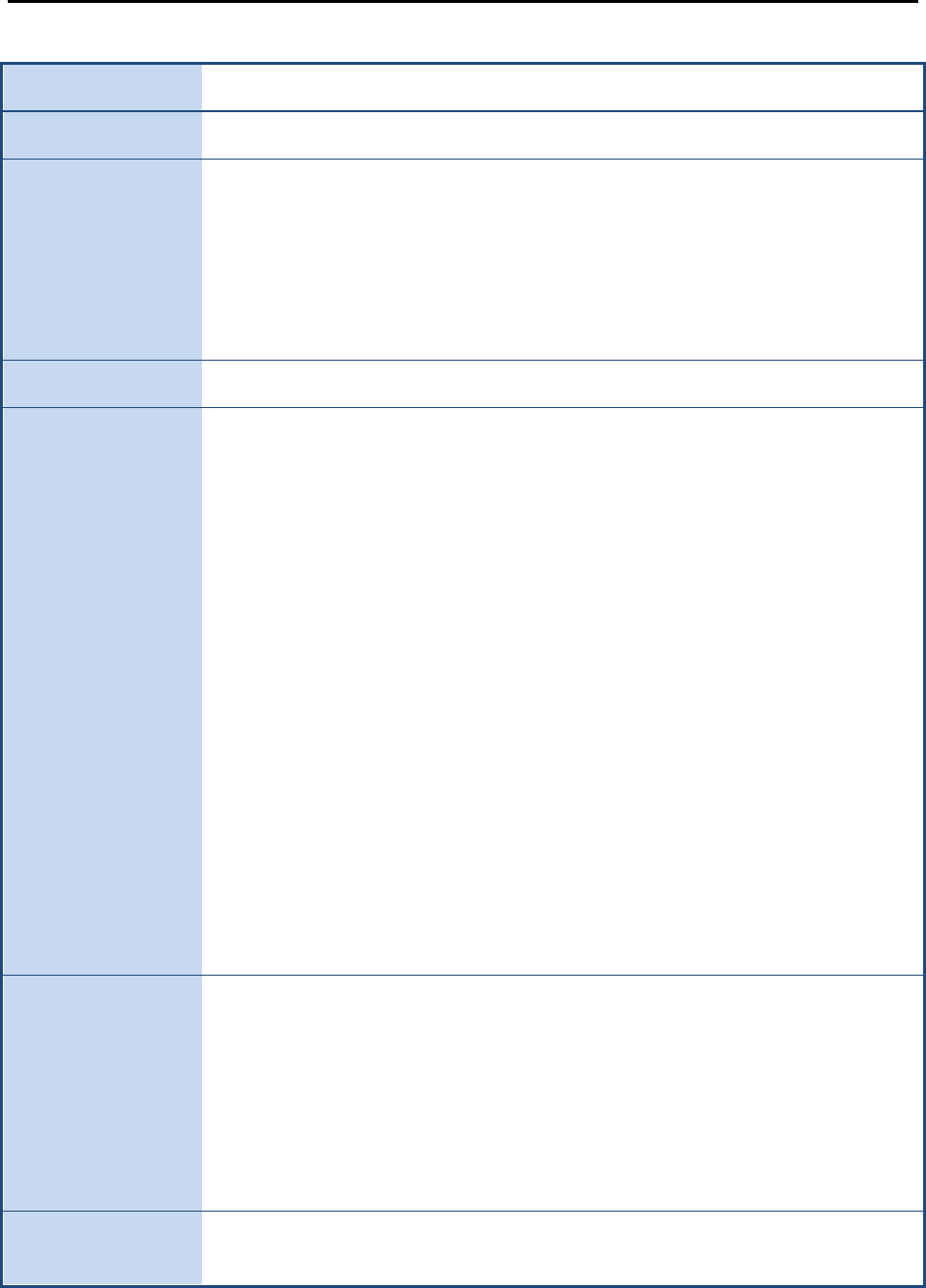
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 11 114
Table 4: A Process for Collecting Data
When? Ask for data early — ideally, during admission or registration
Who? Properly trained admissions or reception staff could collect data
What will you tell
individuals?
Before obtaining information, develop a script to communicate that:
o This information is important.
o It will be used to improve care and services and to prevent
discrimination.
o This information will be kept confidential.
In addition, address any concerns up front and clearly.
How? Individual self-report — select their own race, ethnicity, language, etc.
What information
will you collect?
(Individual Data)
o Race
o Ethnicity
o Nationality
o Nativity
o Ability to speak English
o Language(s) other than English spoken
o Preferred spoken/written languages or other mode of communication
o Age
o Gender
o Sexual orientation
o Gender identity
o Income
o Education
o Informed of right to interpreter services
o Request for, and/or use of, interpreter services
o Treatment history
o Medical history
o Outcome data (service type, utilization, length of stay)
o Client satisfaction
See also aforementioned HHS Data Collection Standards
What information
will you collect?
(Staff Data)
o Race
o Ethnicity
o Nationality
o Nativity
o Primary/preferred language
o Gender
o Records of cultural and linguistic competency training participation and
evaluations
Tools to collect
and store data
Use standard collection instruments. Store data in a standard electronic format.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 11 115
Training
Provide ongoing data training and evaluation to staff
(Massachusetts Department of Public Health, Office of Health Equity, 2009)
Adapted from the Health Research and Evaluation Trust Health Disparities Toolkit (Hasnain-Wynia et al., 2007)
Resources
Asset-Based Community Development Institute.
(2009). Retrieved from http://www.abcdinstitute.org/
Baker, Q. E., Davis, D. A., Gallerani, R., Sanchez, V., Viadro, C., & The Center for the Advancement of
Community Based Public Health. (2000).
An evaluation framework for community health
programs.
Retrieved from
http://www.doh.state.fl.us/COMPASS/documents/Community_Health_Programs_Eval.pdf
Hasnain-Wynia, R., Van Dyke, K., Youdelman, M., Krautkramer, C., Ivey, S., Gilchick, R., Kaleba, E., &
Wynia, M. K. (2010). Barriers to collecting patient race, ethnicity and primary language data in
physician practices: An exploratory study.
Journal of the National Medical Association, 102
(9),
769–775.
Sharpe, P. A., Greaney, M. L., Lee, P. R., & Royce, S. W. (2000). Assets-oriented community assessment.
Public Health Reports, 115,
205–211. Retrieved from
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1308712/pdf/pubhealthrep00022-0103.pdf
U.S. Department of Commerce, Census Bureau. (n.d.).
American factfinder.
Retrieved from
http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2011).
CAHPS cultural competence item set.
Retrieved from https://www.cahps.ahrq.gov/surveys-
guidance/item-sets/cultural-competence.aspx
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2011).
CAHPS item set for addressing health literacy.
Retrieved from
https://www.cahps.ahrq.gov/surveys-guidance/item-sets/health-literacy.aspx
U.S. Department of Health and Human Services, Office of Minority Health. (2011).
Final data collection
standards for race, ethnicity, primary language, sex, and disability status required by Section
4302 of the Affordable Care Act.
Retrieved from
http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlid=208
U.S. Department of Health and Human Services. (2011).
Improving data for the LGBT community.
Retrieved from http://www.healthcare.gov/news/factsheets/2011/06/lgbt06292011a.html
Wynia, M., Hasnain-Wynia, R., Hotze, T. D., & Ivey, S. L. (2011).
Collecting and using race, ethnicity and
language data in ambulatory settings: A white paper with recommendations from the
Commission to End Health Care Disparities.
Retrieved from American Medical Association
website: http://www.ama-assn.org/resources/doc/public-health/cehcd-redata.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 11 116
Additional resources can be found in Appendix E and at www.ThinkCulturalHealth.hhs.gov.
Bibliography
Bilheimer, L. T., & Klein, R. J. (2010). Data and measurement issues in the analysis of health disparities.
Health Services Research, 45,
1489–1507. doi:10.1111/j.1475-6773.2010.01143.x
Fiscella, K. (2011). Eliminating disparities in health care through quality improvement. In R. A. Williams
(Ed.),
Healthcare disparities at the crossroads with healthcare reform
(pp. 231–267). New York,
NY: Springer.
Hasnain-Wynia, R., & Baker, D. W. (2006). Obtaining data on patient race, ethnicity, and primary
language in health care organizations: Current challenges and proposed solutions.
Health
Services Research, 41,
1501–1518. doi:10.1111/j.1475-6773.2006.00552.x
Hasnain-Wynia, R., Pierce, D., Haque, A., Hedges Greising, C., Prince, V., & Reiter, J. (2007).
Health
Research and Educational Trust disparities toolkit.
Retrieved from http://www.hretdisparities.org/
Hasnain-Wynia, R., Pierce, D., & Pittman, M. A. (2004).
Who, when, and how: The current state of race,
ethnicity, and primary language data collection in hospitals
(Commonwealth Fund Publication No.
726). Retrieved from The Commonwealth Fund website:
http://www.commonwealthfund.org/~/media/Files/Publications/Fund%20Report/2004/May/Who
%20%20When%20%20and%20How%20%20The%20Current%20State%20of%20Race%20%2
0Ethnicity%20%20and%20Primary%20Language%20Data%20Collection%20in%20Ho/hasnain
%20wynia_whowhenhow_726%20pdf.pdf
Higgins, P. C., & Taylor, E. F. (2009).
Measuring racial and ethnic disparities in health care: Efforts to
improve data collection.
Retrieved from Mathematica Policy Research website:
http://www.mathematica-mpr.com/pdfs/health/DisparitiesHealthcare.pdf
Institute of Medicine. (2009).
Race, ethnicity, and language data: Standardization for health care quality
improvement
. Retrieved from http://iom.edu/Reports/2009/RaceEthnicityData.aspx
Jorgensen, S., Thorlby, R., Weinick, R. M., & Ayanian, J. Z. (2010). Responses of Massachusetts hospitals
to a state mandate to collect race, ethnicity and language data from patients: A qualitative study.
BMC Health Services Research, 10,
352–359. doi:10.1186/1472-6963-10-352
Lurie, N., & Fremont, A. (2006). Looking forward: Cross-cutting issues in the collection and use of
racial/ethnic data.
Health Services Research, 41,
1519–1533. doi:10.1111/j.1475-
6773.2006.00553.x
Massachusetts Department of Public Health, Office of Health Equity. (2009).
Making CLAS happen: Six
areas for action
. Retrieved from http://www.mass.gov/eohhs/provider/guidelines-
resources/services-planning/workforce-development/health-equity/clas/making-clas-happen.html

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 11 117
National Research Council. (2009).
Principles and practices for a federal statistical agency
(4
th
ed.).
Retrieved from http://www.nap.edu/catalog.php?record_id=12564
Nerenz, D. R. (2005). Health care organizations’ use of race/ethnicity data to address quality disparities.
Health Affairs, 24,
409–416. doi:10.1377/hlthaff.24.2.409.
Robert Wood Johnson Foundation. (2004).
Key findings from a national survey conducted among adults
who have health care coverage on behalf of the Robert Wood Johnson Foundation on the issue
of disparities in health care.
Retrieved from
http://www.rwjf.org/files/newsroom/POSfullMemo.pdf
U.S. Department of Health and Human Services. (2011a).
Implementation guidance on data collection
standards for race, ethnicity, sex, primary language, and disability status.
Retrieved from
http://aspe.hhs.gov/datacncl/standards/ACA/4302/index.pdf
U.S. Department of Health and Human Services. (2011b).
HHS action plan to reduce racial and ethnic
disparities: A nation free of disparities in health and health care
. Retrieved from
http://minorityhealth.hhs.gov/npa/files/Plans/HHS/HHS_Plan_complete.pdf
U.S. Department of Health and Human Services. (2012).
Lesbian, gay, bisexual, and transgender health
.
Retrieved from http://healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=25
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2011).
New communication protocols, inclusive policies, and ongoing training lead to culturally
competent care for lesbian, gay, bisexual, and transgender patients.
Retrieved from
http://www.innovations.ahrq.gov/content.aspx?id=2737
U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion.
(2000).
Healthy people 2010: Understanding and improving health.
Retrieved from
http://www.healthypeople.gov/2010/Document/tableofcontents.htm#under
U.S. Department of Health and Human Services, Office of Minority Health. (2001).
National standards for
culturally and linguistically appropriate services in health care: Final report.
Retrieved from
http://minorityhealth.hhs.gov/assets/pdf/checked/finalreport.pdf
Wynia, M. K., Ivey, S. L., & Hasnain-Wynia, R. (2010). Collection of data on patients' race and ethnic
group by physician practices.
New England Journal of Medicine, 362,
846–850.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 12 118
Standard 12: Conduct Assessments of Community Health Assets
and Needs
Standard 12
The National CLAS Standards are intended to advance health equity, improve quality, and help eliminate
health care disparities by establishing a blueprint for health and health care organizations to:
Conduct regular assessments of community health assets and needs and use the results to plan and
implement services that respond to the cultural and linguistic diversity of populations in the service area.
Purpose
The purposes of conducting assessments of community health assets and needs are:
o To determine the service assets and needs of the populations in the service areas (needs
assessment)
o To identify all of the services available and not available to the populations in the service areas
(resource inventory and gaps analysis)
o To determine what services to provide and how to implement them, based on the results of the
community assessment
o To ensure that health and health care organizations obtain demographic, cultural, linguistic, and
epidemiological baseline data (quantitative and qualitative) and update the data regularly to
better understand the populations in their service areas
Please refer to the glossary in Appendix A for definitions of the key terms used.
Components of the Standard
Conduct Regular Assessments of Community Health Assets and Needs
An effective model for knowing and understanding one’s community and how best to serve it is a
community services assessment.
A community services assessment is composed of three parts (AED Center on AIDS & Community Health,
2005):
o Needs Assessment

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 12 119
o Resource Inventory
o Gaps Analysis
Community services assessments are currently used in various areas of public and community health,
including AIDS prevention (HHS CDC, 2003). The cultural knowledge they provide can help organizations
better utilize community assets and develop or adapt existing services to better meet community needs.
A community services assessment helps an organization understand its community by identifying
individuals from the populations in the service area who may need specific, tailored interventions due to
cultural or linguistic differences. A community services assessment may also aid in the development of
culturally and linguistically appropriate services by helping to identify and define the dynamics of
difference between organizations and the populations they serve, especially those involving health
beliefs, attitudes toward health and health care, and perceptions of effective health communication. It
also allows an organization to avoid duplication in the creation or promotion of services via identification
of the assets already utilized in the community. These data can be used for the development or
adaptation of services to address unmet needs (e.g., incorporating assets in the development or
adaptation of services) and to provide a framework within which services can be evaluated.
Once key stakeholders from the populations in the service area are identified, an organization will be
better able to establish partnerships with community-based organizations, faith-based organizations, and
nonprofit or nongovernmental organizations within the service area. These partnerships will not only
improve access to and utilization of services through improved awareness, but they may also increase an
individual’s perceived satisfaction with those services. Community support and insight facilitate the
implementation of culturally and linguistically appropriate services and policies.
Plan and implement services that respond to the cultural and linguistic diversity of
populations in the service area
Conducting a community needs assessment should be just the first step in a comprehensive effort to
engage local communities in organizational planning and operations (see Standard 13). Data and
information collected from regular community assessments can be used to develop a comprehensive
profile of the populations in the service area, which could have significant demographic and
epidemiological value. Such a profile would help organizations, providers, and policymakers develop
appropriate services and evaluate access to and utilization of those services over time. In addition, data
from this profile could be used to generate more specific profiles (e.g., linguistic or geographic profiles)
that could be used to inform targeted service development and service delivery plans.
According to The Joint Commission’s
Advancing Effective Communication, Cultural Competence, and
Patient- and Family-Centered Care: A Roadmap for Hospitals
(2010), health and health care organizations
should develop and maintain community profiles to:
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 12 120
o Allow organizations to plan for the services necessary to meet individuals’ and groups’ needs
o Identify and respond to changes in the demographics of the surrounding community
o Identify potential disparities in care or services
o Plan for services to meet unique individual needs
o Identify language needs of the population
o Provide appropriate language services to meet those needs
Strategies for Implementation
The following are possible implementation strategies for assessing community health assets and needs.
o Partner with other organizations to negotiate a data sharing agreement, which could facilitate the
linking of different types of data.
o Collaborate with other organizations and stakeholders in data collection, analysis, and reporting
efforts to increase data reliability and validity.
o Conduct focus groups with individuals in the community (QSource, 2005).
o Review demographic data collected with local health and health care organizations (QSource,
2005).
o Use multiple sources in the community to collect data, including faith-based organizations, social
workers, and managed care organizations (QSource, 2005).
The HHS Administration for Children and Families’ Head Start initiative recommends the following Outline
for Assessing Community Needs and Resources (HHS Administration for Children and Families, 2008;
University of Kansas, n.d.):
1. Describe the makeup and history of the community to provide a context within which to collect
data on its current concerns.
a. Comment on the types of information that best describe the community (e.g.,
demographic, historical, political, civic participation, key leaders, past concerns,
geographic, assets)
b. Describe the sources of information used (e.g., public records, local people, Internet,
maps, phone book, library, newspaper)
c. Comment on whether there are sufficient resources available to collect this information
(e.g., time, personnel, resources)

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 12 121
d. Describe the methods used to collect descriptive information (e.g., public forums,
listening sessions, focus groups, interviews, surveys, observation)
e. Assess the quality of the information
f. Describe the strengths and difficulties identified
2. Describe what matters to people in the community, including a description of:
a. Issues that people in the community care about (e.g., safety, education, housing, health)
b. How important these issues are to the community (e.g., perceived importance,
consequences for the community)
c. Methods the organization will (did) use to listen to the community (e.g., listening
sessions, public forums, interviews, concerns surveys, focus groups)
3. Describe what matters to key stakeholders, including:
a. Who else cares about the issue (the stakeholders) and what they care about
b. What stakeholders want to know about the situation (e.g., who is affected, how many,
what factors contribute to the problem)
c. Prioritized populations and subgroups to whom stakeholders are targeting benefits
d. Methods used to gather information (e.g., surveys, interviews)
4. (For each identified problem/goal) Describe the evidence indicating whether the problem/goal
should be a priority issue, including:
a. The community-level indicators related to the issue (e.g., rate of infant deaths or vehicle
crashes)
b. How frequently the problem (or related behavior) occurs (e.g., number of youth
reporting alcohol use in the past 30 days)
c. How many people are affected by the problem and the severity of its effects
d. How feasible it is to address the issue
e. Possible impact and/or consequences of addressing the problem/goal
5. Describe the barriers and resources for addressing the identified issue(s), including:
a. Barriers or resistance to solving the problem or achieving the goal (e.g., denial or
discounting of the problem) and how they can be minimized (e.g., reframing the issue)
b. What resources and assets are available and how the organization can tap into those
resources to address the issue
c. Community context or situation that might make it easier or more difficult to address this
issue
6. (Based on the assessment) Select and state the priority issue (or issues) to be addressed by the
organization.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 12 122
Resources
Asset-Based Community Development Institute.
(2009). Retrieved from http://www.abcdinstitute.org/
Aubel, J. (1999).
Participatory program evaluation manual: Involving program stakeholders in the
evaluation process.
Retrieved from http://www.idrc.ca/uploads/user-
S/10504133390Participatory_Program_Evaluation_Manual.pdf
Baker, Q. E., Davis, D. A., Gallerani, R., Sanchez, V., Viadro, C., & The Center for the Advancement of
Community Based Public Health. (2000).
An evaluation framework for community health
programs.
Retrieved from
http://www.doh.state.fl.us/COMPASS/documents/Community_Health_Programs_Eval.pdf
Clinical and Translational Science Awards Consortium, Community Engagement Key Function Committee
Task Force on the Principles of Community Engagement. (2011).
Principles of community
engagement
(2nd ed.) (National Institutes of Health Publication No. 11-7782). Retrieved from
http://www.atsdr.cdc.gov/communityengagement/pdf/PCE_Report_508_FINAL.pdf
Sharpe, P. A., Greaney, M. L., Lee, P. R., & Royce, S. W. (2000). Assets-oriented community assessment.
Public Health Reports, 115,
205–211. Retrieved from
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1308712/pdf/pubhealthrep00022-0103.pdf
University of Washington, Community-Campus Partnerships for Health. (n.d.).
Community-based
participatory research.
Retrieved from http://depts.washington.edu/ccph/commbas.html
Additional resources can be found in Appendix E and at www.ThinkCulturalHealth.hhs.gov.
Bibliography
AED Center on AIDS & Community Health. (2005).
HIV prevention community planning: An orientation
guide
. Retrieved from
http://www.cdc.gov/hiv/topics/cba/resources/guidelines/Orientation_Final.pdf
The Joint Commission. (2010).
Advancing effective communication, cultural competence, and patient-
and family-centered care: A roadmap for hospitals.
Retrieved from
http://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf
QSource, Underserved Quality Improvement Organization Support Center. (2005).
CLAS Standards
implementation tips.
Retrieved from
http://www.qsource.org/uqiosc/CLAS%20Standards%20Strategies%5B7AUG-2005%5D.pdf
University of Kansas. (n.d.).
Assessing community needs and resources: Outline for assessing community
needs and resources
. Retrieved from
http://ctb.ku.edu/en/dothework/tools_tk_content_page_77.aspx

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 12 123
U.S. Department of Health and Human Services, Administration for Children and Families. (2008).
Outline
for assessing community needs and resources: Assessing community needs and resources
.
Retrieved from http://eclkc.ohs.acf.hhs.gov/hslc/tta-
system/operations/Fiscal/Grants/Community%20Assessment/fiscal_art_00177_090205.html
U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. (2003).
HIV
prevention: Community planning guide
. Retrieved from http://www.cdc.gov/hiv/pubs/hiv-cp.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 13 124
Standard 13: Partner with the Community
Standard 13
The National CLAS Standards are intended to advance health equity, improve quality, and help eliminate
health care disparities by establishing a blueprint for health and health care organizations to:
Partner with the community to design, implement, and evaluate policies, practices, and services to ensure
cultural and linguistic appropriateness.
Purpose
The purpose of partnering with the community is:
o To provide responsive and appropriate service delivery to a community
o To ensure that services are informed and guided by community interests, expertise, and needs
o To increase use of services by engaging individuals and groups in the community in the design
and improvement of services to meet their needs and desires
o To create an organizational culture that leads to more responsive, efficient, and effective services
and accountability to the community
o To empower members of the community in becoming active participants in the health and health
care process
Please refer to the glossary in Appendix A for definitions of the key terms used.
Components of the Standard
Partner with the community
Community partnerships are an essential component in the provision of cultural and linguistic
competency. Only through meaningful community partnerships can an organization truly understand the
individual needs of the diverse population it serves, appropriately allocate resources, and develop an
accountable system that provides equitable culturally and linguistically appropriate care and services
(Douglas et al., 2009; Wu & Martinez, 2006). In addition, community engagement has been found to be
strongly correlated with higher patient-reported quality of care and trust (Wynia et al., 2010).
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 13 125
Design, implement, and evaluate policies, practices, and services to ensure cultural and
linguistic appropriateness
Input from individuals in the community is essential to planning, implementing, and improving services.
Community input provides health and health care organizations with the opportunity to learn about and
understand their reputation in the community. Designing, implementing, and evaluating services, all of
which have been informed by community input, is particularly useful in improving the organization’s reach
and services. If an organization communicates messages that individuals in the community view as
unrealistic — for example, advice to take a daily walk when there are concerns about neighborhood
safety — the messages may not result in the desired behavior change and will be unproductive.
Organizations will be more effective and will ultimately experience cost savings if they consider
community input.
Strategies for Implementation
The following are implementation strategies for partnering with the community:
o Partner with local culturally diverse media to promote better understanding of available care and
services and of appropriate routes for accessing services among all community members (Wilson-
Stronks & Galvez, 2007).
o Build coalitions with community partners to increase reach and impact in identifying and creating
solutions. For example:
•
Work on joint steering committees and coalitions.
•
Sponsor or participate in health fairs, cultural festivals, and celebrations.
•
Offer education and training opportunities.
o Convene town hall meetings, hold community forums, and/or conduct focus groups (Prevention
by Design, 2006).
o Develop opportunities for capacity building initiatives, action research, involvement in service
development, and other activities to empower the community (Equality and Human Rights
Commission, 2009).
o Collaborate to reach more people, to share information and learn, and to improve services. Work
with partners to advertise job openings, identify interpreting resources, and organize health
promotion activities. Successful partnerships benefit all.
In addition, the following professionals and volunteers may facilitate communication between an
organization and the community it serves:
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 13 126
o Cultural brokers are individuals from the community who can serve as a bridge between an
organization and people of different cultural backgrounds. Cultural brokers should be familiar
with the health system and with the community in which they live and/or from where they
originated. They can become a valuable source of cultural information and serve as mediators in
conflicts and as agents for change (Massachusetts Department of Public Health, 2009).
o Promotores de salud/community health workers are volunteer community members and paid
front-line public health workers who are trusted members of the community served or have an
unusually close understanding of that community. They generally share the ethnicity, language,
socio-economic status, and life experiences of the community members. These social attributes
and trusting relationships enable community health workers to serve as liaisons, links, or
intermediaries between health and social services and the community to facilitate access to and
enrollment in services and improve the quality and cultural competency of services (HHS OMH,
2011).
Resources
Association of the Bar of the City of New York. (n.d.).
Diversity committees that make a difference.
Retrieved from
http://www.akcsystems.com/test3/images/stories/pdfs/Diversity%20Committee%20Notes%20Art
icle10_2004.pdf
Baker, S., Conrad, D., Béchamps, M., & Barry M. (2002).
Healthy people toolkit 2010: A field guide to
health planning.
Retrieved from Public Health Foundation website:
http://www.phf.org/resourcestools/Documents/HP2010Toolkit2002.pdf
Clinical and Translational Science Awards Consortium, Community Engagement Key Function Committee
Task Force on the Principles of Community Engagement. (2011).
Principles of community
engagement
(2nd ed.) (National Institutes of Health Publication No. 11-7782). Retrieved from
http://www.atsdr.cdc.gov/communityengagement/pdf/PCE_Report_508_FINAL.pdf
Institute for Patient- and Family-Centered Care. (2011).
Tools to foster the collaboration with patient and
family advisors.
Retrieved from http://www.ipfcc.org/tools/downloads-tools.html
Leonhardt, K., Bonin, D., & Pagel, P. (2008).
Guide for developing a community-based patient safety
advisory council
(AHRQ Publication No. 08-0048). Retrieved from
http://www.ahrq.gov/qual/advisorycouncil/advisorycouncil.pdf
Schillinger, D. (2010).
An introduction to effectiveness, dissemination and implementation research: A
resource manual for community-engaged research.
Retrieved from
http://accelerate.ucsf.edu/files/CE/edi_introguide.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 13 127
Summit Health Institute for Research and Education. (2004).
Building coalitions among communities of
color: A multicultural approach.
Retrieved from http://www.shireinc.org/wp-
content/files/Building_Coalitions_among_Communities_of_Color.pdf
Torres, G., & Margolin, F. (2003).
The collaboration primer: Proven strategies, considerations, and tools
to get you started.
Retrieved from Health Research and Educational Trust website:
http://www.hret.org/upload/resources/collaboration-primer.pdf
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2011).
CAHPS cultural competence item set.
Retrieved from https://www.cahps.ahrq.gov/surveys-
guidance/item-sets/cultural-competence.aspx
Additional resources can be found in Appendix E and at www.ThinkCulturalHealth.hhs.gov.
Bibliography
Douglas, M. K., Pierce, J. U., Rosenkoetter, M., Callister, L. C., Hattar-Pollara, M., Lauderdale, J., &
Pacquiao, D. (2009). Standards of practice for culturally competent nursing care: A request for
comments.
Journal of Transcultural Nursing, 20,
257–269.
Equality and Human Rights Commission. (2009).
Good practice in community engagement from an
equality perspective
. Retrieved from
http://www.equalityhumanrights.com/uploaded_files/good_practice_in_community_engagement.
pdf
Massachusetts Department of Public Health, Office of Health Equity. (2009).
Making CLAS happen: Six
areas for action.
Retrieved from http://www.mass.gov/eohhs/provider/guidelines-
resources/services-planning/workforce-development/health-equity/clas/making-clas-happen.html
Prevention by Design. (2006).
Community engagement strategies: Tip sheet
. Retrieved from
http://socrates.berkeley.edu/~pbd/pdfs/Community_Engagement_Strategies.pdf
U.S. Department of Health and Human Services, Office of Minority Health. (2011).
Definition of
promotoras de salud
. Retrieved from
http://minorityhealth.hhs.gov/templates/content.aspx?lvl=2&lvlid=207&ID=8930
Wilson-Stronks, A., & Galvez, E. (2007).
Hospitals, language, and culture: A snapshot of the nation.
Retrieved from The Joint Commission website:
http://www.jointcommission.org/assets/1/6/hlc_paper.pdf
Wu, E., & Martinez, M. (2006).
Taking cultural competency from theory to action
(Commonwealth Fund
Publication No. 964). Retrieved from The Commonwealth Fund website:
http://www.commonwealthfund.org/usr_doc/Wu_takingcultcomptheoryaction_964.pdf

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 13 128
Wynia, M. K., Johnson, M., McCoy, T. P., Passmore Griffin, L., & Osborn, C. Y. (2010). Validation of an
organizational communication climate assessment toolkit.
American Journal of Medical Quality,
25
(6), 436–443. doi:10.1177/1062860610368428
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 14 129
Standard 14: Create Conflict and Grievance Resolution Processes
Standard 14
The National CLAS Standards are intended to advance health equity, improve quality, and help eliminate
health care disparities by establishing a blueprint for health and health care organizations to:
Create conflict and grievance resolution processes that are culturally and linguistically appropriate to
identify, prevent, and resolve conflicts or complaints.
Purpose
The purposes of creating conflict and grievance resolution processes that are culturally and linguistically
appropriate are:
o To facilitate open and transparent two-way communication and feedback mechanisms between
individuals and organizations
o To anticipate, identify, and respond to cross-cultural needs
o To meet federal and/or state level regulations that address topics such as grievance procedures,
the use of ombudspersons, and discrimination policies and procedures
Please refer to the glossary in Appendix A for definitions of the key terms used.
Components of the Standard
Create conflict and grievance resolution processes that are culturally and linguistically
appropriate
As documented in the HHS Agency for Healthcare Research and Quality’s 2011 National Healthcare
Quality Report and National Healthcare Disparities Report, access to quality health care remains
suboptimal, particularly for minority and low-income groups (2012). One contributing factor of health
disparities is the existence of discriminatory, inequitable practice (IOM, 2003). Culturally and linguistically
appropriate conflict and grievance resolution processes address the discrimination and unfair treatment
— actual and perceived — of diverse populations. Discrimination based on race, ethnicity, sex, age,
socioeconomic status, sexual orientation, gender identity, and other characteristics impede the provision
of quality care and services, making culturally and linguistically competent conflict prevention and
resolution a vital part of advancing health equity.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 14 130
Individuals from diverse backgrounds may encounter situations in which their needs and preferences are
not accommodated or respected by the organization or its staff. These situations may range from
differences related to informed consent and advance directives, to difficulty in accessing services or
denial of services, to discriminatory treatment (HHS OMH, 2001). While personal preferences for care
should be accommodated as much as possible and equitable nondiscriminatory treatment should be
guaranteed, it is inevitable that individuals will have conflicts and grievances. To address this,
organizations should ensure that all staff members are trained to recognize and prevent these potential
conflicts and must develop a method through which individuals can provide feedback. All individuals must
then be informed about, and have access to, these feedback procedures that cover all aspects of their
interaction with the organization (HHS OMH, 2001).
Organizations should anticipate and be responsive to the differences that arise between individuals and
the organization and its staff. This responsiveness may be achieved by integrating principles of cultural
sensitivity into existing feedback procedures, as well as into policies, programs, and committees charged
with responsibility for patient relations and legal or ethical issues. When existing structures are
inadequate, new approaches may need to be developed.
As addressed in Standard 4, governance, leadership, and staff should be trained in cultural and linguistic
competency so that they are prepared to respond appropriately to feedback received by individuals or
groups in their service area. Procedural guidelines, courses, and case study analysis can educate staff on
how to listen and respond respectfully. Appropriate training and procedural guidelines will allow staff to
respond to all feedback, including complaints. Organizations should also create programs with an
ombudsperson and a diverse staff to proactively address individuals’ rights and protections. Such a
program can provide another quality feedback loop on the effectiveness of ongoing cultural and linguistic
competency initiatives. The feedback process should be understandable, easily accessible, confidential,
and transparent.
Health and health care organizations should not assume that a lack of conflict or complaints equates to
satisfaction with services or care provided. Individuals may have fears or cultural beliefs that inhibit
criticism or may not know that they have the right to provide feedback. Individuals may also believe that
feedback will be disregarded by the organization. Thus, in anticipation of individuals who are not
comfortable with expressing or acting upon their own concerns, the organization should have both formal
and informal procedures to solicit feedback.
Strategies for Implementation
The following are possible implementation strategies for creating conflict and grievance resolution
processes that are culturally and linguistically appropriate:
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 14 131
o Provide cross-cultural communication training, including how to work with an interpreter, and
conflict resolution training to staff who handle conflicts, complaints, and feedback.
o Provide notice in signage, translated materials, and other media about the right of each individual
to provide feedback, including the right to file a complaint or grievance.
o Develop a clear process to address instances of conflict and grievance that includes follow-up and
ensures that the individual is contacted with a resolution and next steps (QSource, 2005).
o Obtain feedback via focus groups, community council or town hall meetings, meetings with
community leaders, suggestion and comment systems, open houses, and/or listening sessions.
o Hire patient advocates or ombudspersons (QSource, 2005).
o Include oversight of conflict and grievance resolution processes to ensure their cultural and
linguistic appropriateness as part of the organization’s overall quality assurance program.
Resources
Dator, J. (1991). Culturally-appropriate dispute resolution techniques and the formal judicial system in
Hawaii. A report to the State Justice Institute. Retrieved from
http://www.futures.hawaii.edu/publications/courts/CultAppropAD1991.pdf
DuPraw, M., & Axner, M. (1997). Working on common cross-cultural communication challenges.
Retrieved from http://www.pbs.org/ampu/crosscult.html
Lahey Clinic Foundation. (2012). Retrieved from http://www.lahey.org/
LeBaron, M. (1998). Mediation and multicultural reality. Retrieved from
http://www.gmu.edu/programs/icar/pcs/lebaron.htm
Mind Tools. (n.d.). Conflict resolution: Resolving conflict rationally and effectively. Retrieved from
http://www.mindtools.com/pages/article/newLDR_81.htm
National Center for Cultural Competence, Georgetown University Center for Child and Human
Development, Georgetown University Medical Center. (2004). Bridging the cultural divide in
health care setting: The essential role of cultural broker programs. Retrieved from
http://gucchd.georgetown.edu/products/CulturalBrokerGuide_English.pdf
Rogers, S., & Vilhena, B. (2005). Benchmarking patient complaints data across Ontario hospitals:
University Health Network invites collaboration [Online case study]. Healthcare Quarterly, 8, 82–
84. Retrieved from http://www.longwoods.com/product/download/code/17728
San Francisco Department of Public Health. (n.d.). Retrieved from http://www.sfdph.org/dph/default.asp
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 14 132
Townsend, J. R. (2011). Creating a culturally and politically appropriate dispute resolution model:
Working in Indian country. RCAC's Rural Review, 28(3), 1–7. Retrieved from
http://www.rcac.org/assets/white-papers/CreatingACulturally.pdf
University of Colorado Conflict Information Consortium. (n.d.). Retrieved from
http://conflict.colorado.edu/
Additional resources can be found in Appendix E and at www.ThinkCulturalHealth.hhs.gov.
Bibliography
Institute of Medicine. (2003).
Unequal treatment: Confronting racial and ethnic disparities in health care.
Retrieved from http://www.nap.edu/openbook.php?record_id=10260&page=R1
QSource, Underserved Quality Improvement Organization Support Center. (2005).
CLAS Standards
implementation tips.
Retrieved from
http://www.qsource.org/uqiosc/CLAS%20Standards%20Strategies%5B7AUG-2005%5D.pdf
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2012).
2011 national healthcare disparities report
(AHRQ Publication No. 12-0006). Retrieved from
http://www.ahrq.gov/qual/measurix.htm#quality
U.S. Department of Health and Human Services, Office of Minority Health. (2001).
National standards for
culturally and linguistically appropriate services in health care: Final report.
Retrieved from
http://minorityhealth.hhs.gov/assets/pdf/checked/finalreport.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 15 133
Standard 15: Communicate the Organization’s Progress in
Implementing and Sustaining CLAS
Standard 15
The National CLAS Standards are intended to advance health equity, improve quality, and help eliminate
health care disparities by establishing a blueprint for health and health care organizations to:
Communicate the organization’s progress in implementing and sustaining CLAS to all stakeholders,
constituents, and the general public.
Purpose
The purposes of communicating the organization’s progress in implementing and sustaining CLAS to all
stakeholders, constituents, and the general public are:
o To convey information to intended audiences about efforts and accomplishments in meeting the
National CLAS Standards
o To learn from other organizations about new ideas and successful approaches to implementing
the National CLAS Standards
o To build and sustain communication on CLAS priorities and foster trust between the community
and the service setting
o To meet community benefits and other reporting requirements, including accountability for
meeting health care objectives in addressing the needs of diverse individuals or groups
Please refer to the glossary in Appendix A for definitions of the key terms used.
Components of the Standard
Communicate the organization’s progress in implementing and sustaining CLAS
Communicating to all stakeholders, constituents, and the general public an organization’s efforts to
implement and sustain the National CLAS Standards can serve many purposes. Communication allows an
organization to share its accomplishments in integrating culturally and linguistically appropriate services
in accordance with the National CLAS Standards. It can also help institutionalize the National CLAS
Standards by prompting the organization to regularly focus on the extent to which it has implemented
each Standard, thereby helping to keep the organization accountable. Communicating the organization’s

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 15 134
progress also serves as a mechanism for organizations to learn from each other concerning new ideas
and promising practices for implementing CLAS.
Organizations may exercise latitude in the information they make available and the means by which they
report it to their stakeholders, constituents, and the general public. Examples of possible strategies are
described in the following section. An organization that wishes to provide information can report one or
more of the following: the results of organizational assessments (Standard 10), data collected and
communities served (Standard 11), results of the assessments of the community health assets and needs
(Standard 12), or the various partnerships that have been formed with other organizations from the
community (Standard 13).
Being accountable to the public supports the continuous quality improvement process by documenting
publicly the organization’s ability to provide quality care and services in a culturally and linguistically
appropriate manner. It also informs the organization and community of areas needing improvement.
Communication about CLAS may serve to actively engage the community in assessing an organization’s
service, noting need for improvements, identifying programs that would match its needs, and charting
related progress. Accountability is also important in situations in which an organization is using public
funds to serve the community. Information provided to the public should be relevant, useful, and
understandable to the community. An organization may also communicate CLAS implementation progress
as part of its community benefits and other reporting or accountability requirements.
Strategies for Implementation
The following are implementation strategies for being accountable to the community by presenting to the
public progress in implementing culturally and linguistically appropriate services.
Items on which to report may include (HHS OMH, 2001):
o Demographic data about the populations
o Utilization and availability statistics related to interpreters and translated materials
o Level of staff training in cultural and linguistic competency
o CLAS-related expenditures and cost-benefit data
o Assessment results based on activities suggested from Standard 10, community data collected in
accordance with Standard 12, and the number of complaints and their resolution as collected
pursuant to Standard 14

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 15 135
o Results from performance measures, satisfaction ratings, quality improvement and clinical
outcome data analyses, and cost-effectiveness analyses
Strategies for presenting CLAS-related progress include:
o Draft and distribute materials that demonstrate efforts to be culturally and linguistically
responsive (QSource, 2005). The materials should be easy to understand and in accordance with
Standard 8.
o Partner with community organizations to lead discussions about the services provided and
progress made (QSource, 2005); see also Standard 13.
o Create advisory boards to consult with community partners on issues affecting diverse
populations and how best to serve and reach them (National Consensus Panel on Emergency
Preparedness and Cultural Diversity, 2011).
o Engage community-based workers to help craft and deliver messages and implications of data.
Community outreach that is culturally and linguistically tailored and provided by trusted
messengers is central to ensuring messages are received, understood, and adhered to by local
members of the community. Community-based workers are seen as trusted sources of health
information and can help with reaching and educating communities (National Consensus Panel on
Emergency Preparedness and Cultural Diversity, 2011).
o Convene educational forums. Agencies may consider partnering with well-respected and trusted
community-based organizations to host regional educational forums, inviting local community
representatives to participate. Educational forums are intended to provide education, materials,
and information on topics of most concern to communities — whether regarding public health,
public safety, or primary care. At the same time, they include feedback sessions, where
community partners and representatives can assess and evaluate the validity and application of
recommendations, resources, and materials to their communities’ cultural, social, and economic
circumstances (National Consensus Panel on Emergency Preparedness and Cultural Diversity,
2011).
Resources
Clinical and Translational Science Awards Consortium, Community Engagement Key Function Committee
Task Force on the Principles of Community Engagement. (2011).
Principles of community
engagement
(2nd ed.) (National Institutes of Health Publication No. 11-7782). Retrieved from
http://www.atsdr.cdc.gov/communityengagement/pdf/PCE_Report_508_FINAL.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Standard 15 136
National Committee for Quality Assurance. (2011).
Awards: Recognizing innovations in multicultural
health care.
Retrieved from http://www.ncqa.org/tabid/453/Default.aspx
National Consensus Panel on Emergency Preparedness and Cultural Diversity. (2011).
Guidance for
integrating culturally diverse communities into planning for and responding to emergencies: A
toolkit.
Recommendations of the National Consensus Panel on Emergency Preparedness and
Cultural Diversity
(HHS Office of Minority Health Publication No. OMH-NHMA-5-10). Retrieved
from
http://www.hhs.gov/ocr/civilrights/resources/specialtopics/emergencypre/omh_diversitytoolkit.pd
f
Ohmans, P., & Cushing, M. (2000).
Getting the word out: Effective health outreach to cultural
communities.
Retrieved from The Medtronic Foundation website:
http://www.medtronic.com/downloadablefiles/outreach_brochure.pdf
Sandrick, K. (2006). Defining and measuring community benefit.
Trustee, 59
(9), 6–10. Retrieved from
http://www.trusteemag.com/trusteemag_app/jsp/articledisplay.jsp?dcrpath=TRUSTEEMAG/Pubs
NewsArticleGen/data/2006October/0610TRU_CoverStory&domain=TRUSTEEMAG
U.S. Department of Health and Human Services, Health Resources and Services Administration. (2001).
Cultural competence works: Using cultural competence to improve the quality of health care for
diverse populations and add value to managed care arrangements.
Retrieved from
ftp://ftp.hrsa.gov/financeMC/cultural-competence.pdf
Additional resources can be found in Appendix E and at www.ThinkCulturalHealth.hhs.gov.
Bibliography
National Consensus Panel on Emergency Preparedness and Cultural Diversity. (2011). Guidance for
integrating culturally diverse communities into planning for and responding to emergencies: A
toolkit. Recommendations of the National Consensus Panel on Emergency Preparedness and
Cultural Diversity (HHS Office of Minority Health Publication No. OMH-NHMA-5-10). Retrieved
from
http://www.hhs.gov/ocr/civilrights/resources/specialtopics/emergencypre/omh_diversitytoolkit.pd
f
QSource, Underserved Quality Improvement Organization Support Center. (2005). CLAS Standards
implementation tips. Retrieved from
http://www.qsource.org/uqiosc/CLAS%20Standards%20Strategies%5B7AUG-2005%5D.pdf
U.S. Department of Health and Human Services, Office of Minority Health. (2001). National standards for
culturally and linguistically appropriate services in health care: Final report. Retrieved from
http://minorityhealth.hhs.gov/assets/pdf/checked/finalreport.pdf

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix A: Glossary 137
Appendix A: Glossary
Acculturation:
1
The exchange of cultural features that results when groups of individuals having
different cultures come into continuous firsthand contact; the original cultural patterns of either or both
groups may be altered, but the groups remain distinct.
Augmentative and Alternative Communication (AAC) Resources:
2
Systems or devices that
attempt to temporarily or permanently compensate for and facilitate the impairment and disability of
individuals with severe expressive or language comprehension disorders. AAC may be required for
individuals demonstrating impairments in gestural, spoken, and/or written modalities.
Auxiliary Aids and Services:
3
Devices or services that enable effective communication for people with
disabilities. Examples include qualified interpreters, note takers, transcription services, written materials,
assistive listening devices and systems, telephone communication devices for deaf persons, telephone
handset amplifiers, video interpretive services, and open and closed captioning.
Bilingual:
4
A term describing a person who has some degree of proficiency in two languages. A high
level of bilingualism is the most basic of the qualifications of a competent interpreter but, by itself, does
not ensure the ability to interpret.
Bisexual:
5
One whose sexual or romantic attractions and behaviors are directed at members of both
sexes to a significant degree.
Caregiver:
6
An individual who assists another person who because of physical disability, chronic illness,
or cognitive impairment is unable to perform certain activities on his/her own. So-called informal care can
be offered by family members or friends, often in a home setting. Paid or volunteer professional care, or
so-called formal care, can be obtained at home, in the community, or from institutions such as nursing
facilities or government institutions.
Certification:
7
A process by which a certifying body (usually a governmental or professional
organization) attests to an individual’s qualifications to provide a particular service. Certification calls for
formal assessment using an instrument that has been tested for validity and reliability so that the
certifying body can be confident that the individuals it certifies have the qualifications needed to do the
job.
Certified Interpreter:
8
An interpreter who is certified as competent by a professional organization or
government entity through rigorous testing based on appropriate and consistent criteria. Interpreters
who have had limited training — or have only taken a screening test administered by an employing
health, interpreter, or referral agency — are not considered certified.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix A: Glossary 138
Communication Needs:
9
Difficulty with some aspects of communicating. This difficulty may be minor
and temporary or more complex and long term. The term “needs” refers both to the individual’s needs
and to what society can do to support the individual by examining the individual and the environments in
which he/she interacts.
Requirements of the Americans with Disabilities Act communication needs extend beyond spoken
language capability to include barriers imposed by disabilities affecting hearing, speech, and vision.
10
Community Health Assessment/Community Health Needs Assessment (CHNA):
11
Community
health assessment is a systematic examination of the health status indicators for a given population that
is used to identify key problems and assets in a community. The ultimate goal of a community health
assessment is to develop strategies to address the community’s health needs and identified issues.
Community Needs Assessment:
12
A community needs assessment identifies the strengths and
resources available in the community to meet its needs. The assessment focuses on the capabilities of
the community, including its citizens, agencies, and organizations. It provides a framework for developing
and identifying services and solutions and building communities that support and nurture health and
wellness.
A community needs assessment may be limited to a compilation of demographic data from census
records, results of surveys conducted by others, and informal feedback from community partners.
Alternatively, assessments may be expanded to include focus group discussions, town meetings,
interviews with stakeholders, and telephone or mailed surveys to partnership members and the
community.
Continuous Quality Improvement:
13
The complete process of identifying, describing, and analyzing
strengths and problems and then testing, implementing, learning from, and revising solutions. It relies on
an organizational and/or system culture that is proactive and supports continuous learning. Continuous
quality improvement is firmly grounded in the overall mission, vision, and values of the agency/system.
Perhaps most important, it is dependent upon the active inclusion and participation of staff at all levels of
the agency/system — children, youth, families, and stakeholders — throughout the process.
CLAS: See “Culturally and Linguistically Appropriate Services.”
CLAS Standards: See “National CLAS Standards.”
Cultural Broker:
14
Individuals from the community who serve as bridges between an organization and
people of different cultural backgrounds.
Cultural and Linguistic Competency:
15
The capacity for individuals and organizations to work and
communicate effectively in cross-cultural situations through the adoption and implementation of

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix A: Glossary 139
strategies to ensure appropriate awareness, attitudes, and actions and through the use of policies,
structures, practices, procedures, and dedicated resources that support this capacity.
o
Cultural Competency:
A developmental process in which individuals or institutions achieve
increasing levels of awareness, knowledge, and skills along a cultural competence continuum.
Cultural competence involves valuing diversity, conducting self-assessments, avoiding
stereotypes, managing the dynamics of difference, acquiring and institutionalizing cultural
knowledge, and adapting to diversity and cultural contexts in communities.
o
Linguistic Competency:
The capacity of individuals or institutions to communicate effectively
at every point of contact. Effective communication includes the ability to convey information —
both written and oral — in a manner that is easily understood by diverse groups, including
persons of limited English proficiency, those who have low literacy skills or who are not literate,
those having low health literacy, those with disabilities, and those who are deaf or hard of
hearing.
Culturally and Linguistically Appropriate Services (CLAS):
16
Services that are respectful of and
responsive to individual cultural health beliefs and practices, preferred languages, health literacy levels,
and communication needs and employed by all members of an organization (regardless of size) at every
point of contact.
Culture:
17,18
The integrated pattern of thoughts, communications, actions, customs, beliefs, values, and
institutions associated, wholly or partially, with racial, ethnic, or linguistic groups as well as religious,
spiritual, biological, geographical, or sociological characteristics. Culture is dynamic in nature, and
individuals may identify with multiple cultures over the course of their lifetimes.
Elements of culture include, but are not limited to, the following:
o Age
o Cognitive ability or limitations
o Country of origin
o Degree of acculturation
o Educational level attained
o Environment and surroundings
o Family and household composition
o Gender identity
o Generation
o Health practices, including use of traditional healer techniques such as Reiki and acupuncture.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix A: Glossary 140
o Linguistic characteristics, including language(s) spoken, written, or signed; dialects or regional
variants; literacy levels; and other related communication needs.
o Military affiliation
o Occupational groups
o Perceptions of family and community
o Perceptions of health and well-being and related practices
o Perceptions/beliefs regarding diet and nutrition
o Physical ability or limitations
o Political beliefs
o Racial and ethnic groups include — but are not limited to — those defined by the U.S. Census
Bureau.
o Religious and spiritual characteristics, including beliefs, practices, and support systems related to
how an individual finds and defines meaning in his/her life.
o Residence (i.e., urban, rural, or suburban)
o Sex
o Sexual orientation
o Socioeconomic status
Determinants of Health:
19
Determinants of health care factors that influence health status and
determine health differentials or health inequalities. They are many and varied and include, for example,
natural biological factors, such as age, gender, and ethnicity; behavior and lifestyles, such as smoking,
alcohol consumption, diet, and physical exercise; the physical and social environment, including housing
quality, the workplace, and the wider urban and rural environment; and access to health care.
Effective Communication:
20
The successful joint establishment of meaning wherein patients and
health care providers exchange information, enabling patients to participate actively in their care from
admission through discharge and ensuring that the responsibilities of both patients and providers are
understood. To be truly effective, communication requires a two-way process (expressive and receptive)
in which messages are negotiated until the information is correctly understood by both parties. Successful
communication takes place only when providers understand and integrate the information gleaned from
patients and when patients comprehend accurate, timely, complete, and unambiguous messages from
providers in a way that enables them to participate responsibly in their care.
Ethnicity:
21
The Office of Management and Budget requires federal agencies to use a minimum of two
ethnicities: Hispanic or Latino and Not Hispanic or Latino. Hispanic origin can be viewed as the heritage,
nationality group, lineage, or country of birth of the person or the person’s parents or ancestors before
their arrival in the United States. People who identify their origin as Hispanic, Latino, or Spanish may be
of any race.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix A: Glossary 141
Gay:
22
An attraction and/or behavior focused exclusively or mainly on members of the same sex or
gender identity; a personal or social identity based on one’s same-sex attractions and membership in a
sexual-minority community.
Gender Expression:
23
Characteristics in appearance, personality, and behavior culturally defined as
masculine or feminine.
Gender Identity:
24
One’s basic sense of being a man, woman, or other gender.
Health:
25,26,27
Health encompasses many aspects, including physical, mental, social, and spiritual well-
being. The World Health Organization also notes that health is “not merely the absence of disease or
infirmity.”
Health Care:
28
According to the Health Insurance Portability and Accountability Act of 1996, health care
refers to the care, services, or supplies related to the health of an individual, including but not limited to,
the following:
o Preventive, diagnostic, therapeutic, rehabilitative, maintenance, or palliative care, and counseling,
service, assessment, or a procedure with respect to the physical or mental condition, or
functional status, of an individual or that affects the structure or function of the body; and
o Sale or dispensing of a drug, device, equipment, or other item in accordance with a prescription.
Health Care Disparities:
29
Differences in the receipt of, experiences with, and quality of health care
that are not due to access-related factors or clinical needs, preferences, or appropriateness of
intervention.
Health Care Organization:
30
Any public or private institution involved in any aspect of delivering
health care services.
Health Disparity:
31
A particular type of health difference that is closely linked with social, economic,
and/or environmental disadvantage. Health disparities adversely affect groups of people who have
systematically experienced greater obstacles to health based on their racial or ethnic group; religion;
socio-economic status; gender; age; mental health; cognitive, sensory, or physical disability; sexual
orientation or gender identity; geographic location; or other characteristics historically linked to
discrimination or exclusion.
Health Equity:
32,33
Attainment of the highest level of health for all people. Achieving health equity
requires valuing everyone equally, with focused and ongoing societal efforts to address avoidable
inequalities, historical and contemporary injustices, and the elimination of health and health care
disparities.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix A: Glossary 142
Health Inequality:
34
Difference in health status or in the distribution of health determinants among
different population groups. For example, differences in mobility between elderly people and younger
populations or differences in mortality rates among people from different social classes. It is important to
distinguish between a health inequality and a health inequity. Some health inequalities are attributable to
biological variations or free choice, while others are attributable to the external environment and
conditions mainly outside the control of the individuals concerned. In the first case, it may be impossible
or ethically or ideologically unacceptable to change the health determinants, and so the resultant health
inequality is unavoidable. In the second case, the uneven distribution may be unnecessary and avoidable
as well as unjust and unfair so that the resulting health inequalities also lead to an inequity in health.
Health Inequities:
35
Differences in health status or in the distribution of health determinants among
different population groups.
Health Literacy:
36
The degree to which an individual has the capacity to obtain, process, and
understand basic health information and services needed to make appropriate health decisions.
Health Numeracy:
37
The degree to which an individual has the capacity to access, process, interpret,
communicate, and act on numerical, quantitative, graphical, biostatistical, and probabilistic health
information needed to make effective health decisions.
Health Organization:
38
Any public or private institution addressing individual or community health and
well-being.
Individuals and Groups:
39
Patients, clients, or consumers, including accompanying family members,
guardians, or companions, seeking physical, mental, or other health-related services.
Interpreter:
40
An individual who renders a message spoken or signed in one language into a second
language and who abides by a code of professional ethics.
Types of Interpreters:
o
Ad Hoc Interpreter:
41
An untrained individual who is called upon to interpret, such as a family
member interpreting for his/her parents, a bilingual staff member pulled away from other duties
to interpret, or a self-declared bilingual in a hospital waiting room who volunteers to interpret.
Also called a chance interpreter or lay interpreter.
o
Bilingual Provider:
42
An individual with proficiency in more than one language, enabling the
person to provide services directly to limited English proficient patients in their non-English
language.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix A: Glossary 143
o
Bilingual Worker/Employee:
43
An employee who is a proficient speaker of two languages and
who may provide direct services in both languages but who, without additional training, is not
qualified to serve as an interpreter.
o
Dual-Role Interpreter:
44
A bilingual employee in health care who has been tested for
language skills and trained as a medical interpreter and who assumes the task of part-time
medical interpreting willingly.
o
Qualified Interpreter:
45
An individual who has been assessed for professional skills,
demonstrates a high level of proficiency in at least two languages, and has the appropriate
training and experience to interpret with skill and accuracy while adhering to the National Code of
Ethics and Standards of Practice published by the National Council on Interpreting in Health Care.
Interpreting:
46
o
(noun)
The process of understanding and analyzing a spoken or signed message and
re-expressing that message faithfully, accurately, and objectively in another language, taking the
cultural and social context into account. The purpose of interpreting is to enable communication
between two or more individuals who do not speak one another’s languages.
o
(adjective)
Concerning or involved with interpreting. Examples are interpreting services,
interpreting issues.
Types of Interpreting:
o
Community Interpreting:
47
Interpreting that takes place in the course of communication in
the local community among speakers of different languages. The community interpreter may or
may not be a trained interpreter. Community settings include schools, social service agencies,
clinics, legal services, and businesses that serve a diverse clientele.
o
Consecutive Interpreting:
48
A highly complex cognitive activity that requires the interpreter to
listen, analyze, comprehend, convert, edit, and reproduce the original message, after the speaker
or signer pauses, in a specific social context. Consecutive interpretation is likely to take longer
than simultaneous, because the interpreter does not interpret while the speaker or signer is
speaking or signing.
o
Face-to-Face Interpreting:
49
Interpreting in which the interpreter is present, in person, with
both, or at least one, of the persons for whom interpreting is provided.
o
First-Person Interpreting:
50
The promotion by the interpreter of direct communication
between the principal parties in the interaction through the use of direct utterances of each of

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix A: Glossary 144
the speakers, as though the interpreter were the voice of the person speaking, albeit in the
language of the listener. For example, if the patient says, “My stomach hurts,” the interpreter
says (in the second language), “My stomach hurts,” not “She says her stomach hurts.”
o
Health Care Interpreting:
51
Interpreting that takes place in health care settings of any sort,
including doctors’ offices, clinics, hospitals, home health visits, mental health clinics, and public
health presentations. Typically, the setting is an interview between a health care provider
(doctor, nurse, lab technician) and a patient (or the patient and one or more family members).
o
Simultaneous Interpretation:
52
Highly complex cognitive activity that requires the interpreter
to listen, analyze, comprehend, convert, edit, and reproduce in real time a speaker or signer’s
message while the speaker or signer continues to speak or sign, in a specific social context.
o
Telephone or Telephonic Interpreting:
53
Interpreting carried out remotely, with the
interpreter connected by telephone to the principal parties, typically provided through a
speakerphone or headsets. In health care settings, the principal parties, e.g., doctor and patient,
are normally in the same room, but telephone interpreting can be used to serve individuals who
are also connected to each other only by telephone.
o
Video Remote Interpreting (VRI):
54
An interpreting service that uses video conference
technology over dedicated lines or wireless technology offering a high-speed, wide-bandwidth
video connection that delivers high-quality video images. To ensure that VRI is effective, the
Department of Justice has established performance standards for VRI and requires training for
users of the technology and other individuals involved with its use so that they may quickly and
efficiently set up and operate the VRI system.
Language:
55
While the Office of Budget and Management has not established a list of language
categories, the collection of language data has been pivotal in determining whether there has been
discrimination by “national origin” under Title VI of the Civil Rights Act of 1964, and federal policies state
that “reasonable steps” need to be taken so that persons of limited English proficiency can have
“meaningful access” to programs or activities without charge for language services. Additionally, in 2000,
the Department of Health and Human Services released its National Standards on Culturally and
Linguistically Appropriate Services, which encourages all health care organizations and individual
providers “to make their practices more culturally and linguistically accessible,” including the use of race,
ethnicity, and language data in program assessments and incorporation of these data into health records
and organizational management systems.
Language Assistance Services:
56
Mechanisms used to facilitate communication with individuals who
do not speak English, those who have limited English proficiency, and those who are deaf or hard of

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix A: Glossary 145
hearing. These services can include in-person interpreters, bilingual staff, or remote interpreting systems
such as telephone or video interpreting. Language services also refer to processes in place to provide
translation of written materials or signage, sign language, or braille materials.
Language Concordance:
57
Occurs when the individual seeking services or care and the provider of
said services are able to speak the same primary language well.
Lesbian:
58
A woman who self-identifies as having an emotional, sexual, and/or relational attraction to
other women.
Limited English Proficiency:
59,60
A concept referring to a level of English proficiency that is insufficient
to ensure equal access to public services without language assistance with respect to a particular type of
service, benefit, or encounter.
Meaningful Access:
61
Recipients of federal financial assistance are required to take reasonable steps to
ensure meaningful access to their programs and activities by limited English proficient (LEP) persons.
The HHS Office of Civil Rights Guidance explains that the obligation to provide meaningful access is fact
dependent and starts with an individualized assessment that balances four factors: (1) the number or
proportion of LEP persons eligible to be served or likely to be encountered by the program or grantee; (2)
the frequency with which LEP individuals come into contact with the program; (3) the nature and
importance of the program, activity, or service provided by the recipient to its beneficiaries; and (4) the
resources available to the grantee/recipient and the costs of interpretation/translation services. There is
no one-size-fits-all solution for Title VI compliance with respect to LEP persons, and what constitutes
"reasonable steps" for large providers may not be reasonable where small providers are concerned.
National CLAS Standards:
62
The framework for culturally and linguistically appropriate services issued
by the U.S. Department of Health and Human Services, Office of Minority Health. The National CLAS
Standards are intended to inform, guide, and facilitate practices related to culturally and linguistically
appropriate health service delivery.
Numeracy:
63
A part of literacy that implies a facility with basic probability and numerical concepts.
Plain Language:
64
A strategy for making written and oral information easier to understand;
communication that users can understand the first time they read or hear it. A plain language document
is one in which people can find what they need, understand what they find, and act appropriately on that
understanding.
Primary Language:
65
The language that a limited English proficient individual identifies as the one that
he/she uses to communicate effectively and would prefer to use to communicate with service providers.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix A: Glossary 146
Race:
66
The Department of Health and Human Services and its agencies follow the racial categories
developed by the Office of Management and Budget and used by the U.S. census. These categories
generally reflect a social definition of race recognized in this country and are not an attempt to define
race biologically, anthropologically, or genetically. People may choose to report more than one race to
indicate their racial mixture, such as “American Indian and White.”
People who identify their origin as Hispanic, Latino, or Spanish may be of any race. Racial categories can
include national origin or sociocultural groups.
Information on race is required for many federal programs and is important for making policy decisions,
particularly for civil rights. States use these data to meet legislative redistricting principles. Race data also
are used to promote equal employment opportunities and to assess environmental risks and racial
disparities in health.
Reasonable Steps: For guidance on how to determine whether the steps taken to provide language
access are “reasonable,” providers or organizations should refer to the Department of Health and Human
Services’ Guidance to Federal Financial Assistance Recipients Regarding Title VI Prohibition Against
National Origin Discrimination Affecting Limited English Proficient Persons.
Sex:
67
The Department of Health and Human Services and its agencies follow the sex categories
developed by the Office of Management and Budget and used by the U.S. census. The census
operationalizes sex as “male” or “female.” The census question regarding sex remains unchanged from
the previous census. Information on the sex of individuals is one of the few items obtained in the original
1790 census and in every census since.
It is important to note that sex differs from the concepts of gender, gender identity, and gender
expression.
Sexual Identity:
68
Encompasses attraction, behavior, and identity. Most researchers studying sexual
orientation have defined it operationally in terms of one or more of the following components. Defined in
terms of
behavior
, sexual orientation refers to an enduring pattern of sexual or romantic activity with
men, women, or both sexes. Defined in terms of
attraction
(or desire), it denotes an enduring pattern of
experiencing sexual or romantic feelings for men, women, or both sexes. Identity encompasses both
personal identity and social identity. Defined in terms of
personal identity
, sexual orientation refers to a
conception of the self-based on one’s enduring pattern of sexual and romantic attractions and behaviors
toward men, women, or both sexes. Defined in terms of
social
(or collective)
identity
, it refers to a sense
of membership in a social group based on a shared sexual orientation and a linkage of one’s self-esteem
to that group.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix A: Glossary 147
Social Determinants of Health:
69
The conditions in which people are born, grow, live, work, and age,
including the health system.
Staff:
70
The group of individuals formally affiliated with an institution, including paid employees,
contractors, and unpaid volunteers.
Threshold Population:
71
A threshold population is a linguistic group that makes up 15% or more of a
program’s clients and who share a common language other than English as a primary language. For
example, if program XYZ serves 200 clients, and at least 30 of them speak Haitian-Creole as a primary
language, that group would be considered a threshold population for that program, and Haitian-Creole
would be considered a threshold language. Some programs may target multiple groups and, therefore,
may have multiple threshold populations and threshold languages; some programs may have no
threshold populations.
Traditional Healer Services:
72
The application of knowledge, skills, and practices based on the
experiences indigenous to different cultures. These services are directed towards the maintenance of
health, as well as the prevention, diagnosis, and improvement of physical and mental illness. Examples of
traditional healers include herbalists, faith healers, and practitioners of Chinese or Ayurvedic medicine. In
contrast, allopathic service providers are those trained in western medicine.
Transgender:
73
A person whose gender identity and/or expression is different from that typically
associated with their assigned sex at birth.
Translation:
74
The conversion of a written text into a corresponding written text in a different language.
Translator:
75
A person who translates written texts.
TTY:
76
TTY stands for text telephone. It is also sometimes called a TDD, or telecommunication device for
the deaf. TTY is the more widely accepted term, however, as TTYs are used by many people, not just
people who are deaf.
Vital Documents:
77
For the purposes of ensuring language access, vital documents are written
documents that are “vital” to programs or limited English proficient populations. Examples include signs,
directions, and notices about the availability of interpreter services, client intake forms, and legal
documents (e.g., consent forms, notices of client rights and responsibilities, privacy notices, complaint
forms, grievance policies).
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix A: Glossary 148
Bibliography
1
Kottak, C. P. (2007).
Windows on humanity
(3rd ed.). New York: McGraw Hill.
2
The Joint Commission. (2010).
Advancing effective communication, cultural competence, and patient-
and family-centered care: A roadmap for hospitals
. Retrieved from
http://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf
3
The Joint Commission. (2010).
Advancing effective communication, cultural competence, and patient-
and family-centered care: A roadmap for hospitals
. Retrieved from
http://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf
4
National Council on Interpreting in Health Care. (2008).
The terminology of health care interpreting: A
glossary of terms.
Retrieved from
http://data.memberclicks.com/site/ncihc/NCIHC%20Terms%20Final080408.pdf
5
Institute of Medicine. (2011).
The health of lesbian, gay, bisexual, and transgender people: Building a
foundation for better understanding
. Washington, DC: The National Academies Press.
6
Day, T. (n.d.).
About caregiving.
Retrieved from
http://www.longtermcarelink.net/eldercare/caregiving.htm
7
National Council on Interpreting in Health Care. (2008).
The terminology of health care interpreting: A
glossary of terms.
Retrieved from
http://data.memberclicks.com/site/ncihc/NCIHC%20Terms%20Final080408.pdf
8
National Council on Interpreting in Health Care. (2008).
The terminology of health care interpreting: A
glossary of terms.
Retrieved from
http://data.memberclicks.com/site/ncihc/NCIHC%20Terms%20Final080408.pdf
9
Talking point: The first step for information on children’s communication. (2010). Speech, language and
communication needs. In
Glossary.
Retrieved from
http://www.communicationhelppoint.org.uk/da/Glossary.aspx
10
Institute of Medicine. (2009). Defining language need and categories for collection. In
Race, ethnicity,
and language data: Standardization for health care quality improvement
(pp. 93–126). Retrieved
from http://www.nap.edu/openbook.php?record_id=12696&page=93
11
Consensus Statement from American Public Health Association (APHA), Association of Schools of
Public Health (ASPH), Association of State and Territorial Health Officials (ASTHO), National
Association of County and City Health Officials (NACCHO), National Association of Local Boards of
Health (NALBOH), National Network of Public Health Institutes (NNPHI), and Public Health
Foundation (PHF). (2012). Maximizing the Community Health Impact of Community Health Needs
Assessments Conducted by Tax-exempt Hospitals
http://www.naccho.org/topics/infrastructure/mapp/loader.cfm?csModule=security/getfile&pageID
=228911

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix A: Glossary 149
12
U.S. Department of Health and Human Services, Administration for Children and Families. (n.d.).
Community needs assessment.
Retrieved from
http://www.childwelfare.gov/systemwide/assessment/community.cfm
13
National Child Welfare Resource Center for Organizational Improvement & Casey Family Programs.
(2005).
Using continuous quality improvement to improve child welfare practice.
Retrieved from
http://muskie.usm.maine.edu/helpkids/rcpdfs/CQIFramework.pdf
14
Massachusetts Department of Public Health, Office of Health Equity. (2009).
Making CLAS
happen: Six areas for action.
Retrieved from http://www.mass.gov/eohhs/provider/guidelines-
resources/services-planning/workforce-development/health-equity/clas/making-clas-happen.html
15
Cross, T. L., Bazron, B. J., Dennis, K. W., & Isaacs, M. R. (1989).
Towards a culturally competent
system of care volume I: A monograph on effective services for minority children who are
severely emotionally disturbed.
Washington, DC: Georgetown University Child Development
Center, Child and Adolescent Service System Program Technical Assistance Center.
16
U.S. Department of Health and Human Services, Office of Minority Health. (2001).
National standards
for culturally and linguistically appropriate services in health care: Final report.
Retrieved from
http://www.minorityhealth.hhs.gov/assets/pdf/checked/finalreport.pdf
17
Gilbert, J., Goode, T. D., & Dunne, C. (2007). Cultural awareness. In
Curricula enhancement module
series
. Retrieved from the National Center for Cultural Competence website:
http://www.nccccurricula.info/awareness/index.html
18
U.S. Department of Health and Human Services, Office of Minority Health. (2005).
What is cultural
competency?
Retrieved from
http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlID=11
19
World Health Organization. (2012).
Health impact assessment: Glossary of terms used, A–E.
Retrieved
from http://www.who.int/hia/about/glos/en/index.html
20
The Joint Commission. (2010).
Advancing effective communication, cultural competence, and patient-
and family-centered care: A roadmap for hospitals
. Retrieved from
http://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf
21
Humes, K. R., Jones, N. A., & Ramirez, R. R. (2011, March).
Overview of race and Hispanic origin:
2010.
2010 Census Briefs
. Retrieved from http://www.census.gov/prod/cen2010/briefs/c2010br-
02.pdf
22
Institute of Medicine. (2011).
The health of lesbian, gay, bisexual, and transgender people: Building a
foundation for better understanding
. Washington, DC: The National Academies Press.
23
Institute of Medicine. (2011).
The health of lesbian, gay, bisexual, and transgender people: Building a
foundation for better understanding
. Washington, DC: The National Academies Press.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix A: Glossary 150
24
Bockting, W. O. (1999).
From construction to context: Gender through the eyes of the transgendered
.
SIECUS Report 1(Oct./Nov.):3–7.
25
U.S. Department of Health and Human Services, Indian Health Services. (n.d.).
Our mission
. Retrieved
from http://www.ihs.gov/index.cfm?module=ihsIntro
26
U.S. Department of Health and Human Services, Office of the Surgeon General and National
Action Alliance for Suicide Prevention. (2012).
2012 National strategy for suicide
prevention: Goals and objectives for action
. Retrieved from
http://www.surgeongeneral.gov/library/reports/national-strategy-suicide-
prevention/full_report-rev.pdf
27
World Health Organization. (1946).
Definition of health in preamble to the constitution of the World
Health Organization
. Geneva, Switzerland: World Health Organization.
28
Health Insurance Portability and Accountability Act of 1996, Pub. L. No. 102-168, § 160.103, 110 Stat.
1936 (1996)
29
Institute of Medicine (2003).
Unequal treatment: Confronting racial and ethnic disparities in health
care
. Retrieved from http://www.nap.edu/openbook.php?record_id=10260&page=R1
30
U.S. Department of Health and Human Services, Office of Minority Health. (2001).
National standards
for culturally and linguistically appropriate services in health care: Final report.
Retrieved from
http://www.minorityhealth.hhs.gov/assets/pdf/checked/finalreport.pdf
31
U.S. Department of Health and Human Services, Office of Minority Health, National Partnership for
Action to End Health Disparities. (2011).
Health equity & disparities.
Retrieved from
http://minorityhealth.hhs.gov/npa/templates/browse.aspx?lvl=1&lvlid=34
32
U.S. Department of Health and Human Services, Office of Minority Health, National Partnership for
Action to End Health Disparities. (2011).
Health equity & disparities.
Retrieved from
http://minorityhealth.hhs.gov/npa/templates/browse.aspx?lvl=1&lvlid=34
33
Braveman, P. A. (2003). Monitoring equity in health and healthcare: A conceptual framework.
Journal
of Health, Population, and Nutrition, 21,
181–192.
34
World Health Organization. (2012).
Health impact assessment: Glossary of terms used, F–P.
Retrieved
from http://www.who.int/hia/about/glos/en/index1.html
35
World Health Organization. (2012).
Health impact assessment: Glossary of terms used, F–P.
Retrieved
from http://www.who.int/hia/about/glos/en/index1.html
36
U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion.
(2000). Health communication and health IT. In
Healthy people 2010
. Retrieved from
http://www.healthypeople.gov/2010/hp2020/Objectives/TopicArea.aspx?id=25&TopicArea=Healt
h+Communication+and+Health+IT
37
Golbeck, A. L., Ahlers-Schmidt, C. R., Paschal, A. M., & Dismuke, M. C. (2005). A definition and
operational framework for health numeracy.
American Journal of Preventive Medicine
,
29,
375–
376. doi:10.1016/j.amepre.2005.06.012

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix A: Glossary 151
38
U.S. Department of Health and Human Services, Office of Minority Health. (2001).
National standards
for culturally and linguistically appropriate services in health care: Final report.
Retrieved from
http://www.minorityhealth.hhs.gov/assets/pdf/checked/finalreport.pdf
39
U.S. Department of Health and Human Services, Office of Minority Health. (2001).
National standards
for culturally and linguistically appropriate services in health care: Final report.
Retrieved from
http://www.minorityhealth.hhs.gov/assets/pdf/checked/finalreport.pdf
40
National Health Law Program (2010).
What’s in a word? A guide to understanding interpreting and
translation in health care
. Retrieved from
http://www.healthlaw.org/images/stories/whats_in_a_word_guide.pdf
41
National Council on Interpreting in Health Care. (2008).
The terminology of health care interpreting: A
glossary of terms.
Retrieved from
http://data.memberclicks.com/site/ncihc/NCIHC%20Terms%20Final080408.pdf
42
National Council on Interpreting in Health Care. (2008).
The terminology of health care interpreting: A
glossary of terms.
Retrieved from
http://data.memberclicks.com/site/ncihc/NCIHC%20Terms%20Final080408.pdf
43
National Council on Interpreting in Health Care. (2008).
The terminology of health care interpreting: A
glossary of terms.
Retrieved from
http://data.memberclicks.com/site/ncihc/NCIHC%20Terms%20Final080408.pdf
44
National Council on Interpreting in Health Care. (2008).
The terminology of health care interpreting: A
glossary of terms.
Retrieved from
http://data.memberclicks.com/site/ncihc/NCIHC%20Terms%20Final080408.pdf
45
National Health Law Program (2010).
What’s in a word? A guide to understanding interpreting and
translation in health care
. Retrieved from
http://www.healthlaw.org/images/stories/whats_in_a_word_guide.pdf
46
National Health Law Program (2010).
What’s in a word? A guide to understanding interpreting and
translation in health care
. Retrieved from
http://www.healthlaw.org/images/stories/whats_in_a_word_guide.pdf
47
National Council on Interpreting in Health Care. (2008).
The terminology of health care interpreting: A
glossary of terms.
Retrieved from
http://data.memberclicks.com/site/ncihc/NCIHC%20Terms%20Final080408.pdf
48
ASTM, International. (2007).
Standard guide for language interpretation services
. doi:10.1520/F2089-
01R07
49
National Council on Interpreting in Health Care. (2008).
The terminology of health care interpreting: A
glossary of terms.
Retrieved from
http://data.memberclicks.com/site/ncihc/NCIHC%20Terms%20Final080408.pdf

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix A: Glossary 152
50
National Council on Interpreting in Health Care. (2008).
The terminology of health care interpreting: A
glossary of terms.
Retrieved from
http://data.memberclicks.com/site/ncihc/NCIHC%20Terms%20Final080408.pdf
51
National Council on Interpreting in Health Care. (2008).
The terminology of health care interpreting: A
glossary of terms.
Retrieved from
http://data.memberclicks.com/site/ncihc/NCIHC%20Terms%20Final080408.pdf
52
ASTM, International. (2007).
Standard guide for language interpretation services
. doi:10.1520/F2089-
01R07
53
National Council on Interpreting in Health Care. (2008).
The terminology of health care interpreting: A
glossary of terms.
Retrieved from
http://data.memberclicks.com/site/ncihc/NCIHC%20Terms%20Final080408.pdf
54
U.S. Department of Justice. (2011).
Highlights of the final rule to amend the Department of Justice’s
regulation implementing Title II of the ADA
[Fact sheet]. Retrieved from
http://www.ada.gov/regs2010/factsheets/title2_factsheet.html
55
Institute of Medicine. (2009).
Race, ethnicity, and language data: Standardization for health care
quality improvement
. Retrieved from http://iom.edu/Reports/2009/RaceEthnicityData.aspx
56
The Joint Commission. (2010).
Advancing effective communication, cultural competence, and patient-
and family-centered care: A roadmap for hospitals
. Retrieved from
http://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf
57
Institute of Medicine. (2009). Defining language need and categories for collection. In
Race, ethnicity,
and language data: Standardization for health care quality improvement
(pp. 93–126). Retrieved
from http://www.nap.edu/openbook.php?record_id=12696&page=93
58
U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services
Administration. (2012).
Top Health Issues for LGBT Populations Information & Resource Kit.
(HHS Publication No. (SMA) 12-4684). Retrieved from
http://store.samhsa.gov/shin/content/SMA12-4684/SMA12-4684.pdf
59
The Joint Commission. (2010).
Advancing effective communication, cultural competence, and patient-
and family-centered care: A roadmap for hospitals.
Retrieved from
http://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf
60
U.S. Department of Health and Human Services, Office for Civil Rights. (2004). Limited English
proficiency (LEP). Retrieved from
http://www.hhs.gov/ocr/civilrights/resources/specialtopics/lep/index.html
61
U.S. Department of Health and Human Services, Office for Civil Rights. (2003).
Guidance to federal
financial assistance recipients regarding Title VI and the prohibition against national origin
discrimination affecting limited English proficient persons: Summary
. Retrieved from
http://www.hhs.gov/ocr/civilrights/resources/laws/summaryguidance.html

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix A: Glossary 153
62
U.S. Department of Health and Human Services, Office of Minority Health. (2001).
National standards
for culturally and linguistically appropriate services in health care: Final report.
Retrieved from
http://www.minorityhealth.hhs.gov/assets/pdf/checked/finalreport.pdf
63
Schwartz, L. M., Woloshin, S., Black, W. C., & Welch, H. G. (1997). The role of numeracy in
understanding the benefit of screening mammography.
Annals of Internal Medicine, 127,
966–
972.
64
Plain Language Action and Information Network. (n.d.).
What is plain language?
Retrieved from
http://www.plainlanguage.gov/whatisPL/index.cfm
65
U.S. Department of Health and Human Services. (2008).
Hawaii Department of Human Services
Resolution Agreement.
Retrieved from
http://www.hhs.gov/ocr/civilrights/activities/agreements/hawaiiagree.html
66
U.S. Department of Commerce, Census Bureau. (2011).
Overview of race and Hispanic origin: 2010.
Retrieved from http://www.census.gov/prod/cen2010/briefs/c2010br-02.pdf
67
U.S. Department of Commerce, Census Bureau. (2011, May).
Age and sex composition, 2010
[2010
Census Brief No. C2010BR-03]. Retrieved from
http://www.census.gov/prod/cen2010/briefs/c2010br-03.pdf
68
Institute of Medicine. (2011).
The health of lesbian, gay, bisexual, and transgender people: Building a
foundation for better understanding
. Washington, DC: The National Academies Press.
69
World Health Organization. (2012).
Social determinants of health.
Retrieved from
http://www.who.int/social_determinants/en
70
U.S. Department of Health and Human Services, Office of Minority Health. (2001).
National standards
for culturally and linguistically appropriate services in health care: Final report.
Retrieved from
http://www.minorityhealth.hhs.gov/assets/pdf/checked/finalreport.pdf
71
Massachusetts Department of Public Health, Office of Health Equity. (2009). Glossary and list of
acronyms. In
Making CLAS happen: Six areas for action
(pp. 171–183). Retrieved from
http://www.mass.gov/eohhs/docs/dph/health-equity/clas-appendices-glossary.pdf
72
The World Bank. (2011).
Traditional healer services
. Retrieved from
http://go.worldbank.org/433PVWTQL0
73
U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services
Administration. (2012).
Top Health Issues for LGBT Populations Information & Resource Kit.
(HHS Publication No. (SMA) 12-4684). Retrieved from
http://store.samhsa.gov/shin/content/SMA12-4684/SMA12-4684.pdf
74
National Council on Interpreting in Health Care. (2008).
The terminology of health care interpreting: A
glossary of terms.
Retrieved from
http://data.memberclicks.com/site/ncihc/NCIHC%20Terms%20Final080408.pdf

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix A: Glossary 154
75
National Council on Interpreting in Health Care. (2008).
The terminology of health care interpreting: A
glossary of terms.
Retrieved from
http://data.memberclicks.com/site/ncihc/NCIHC%20Terms%20Final080408.pdf
76
AboutTTY.com: The power of connecting. (n.d.).
What is a TTY?
Retrieved from
http://www.abouttty.com
77
Massachusetts Department of Public Health, Office of Health Equity. (2009). Glossary and list of
acronyms. In
Making CLAS happen: Six areas for action
(pp. 171–183). Retrieved from
http://www.mass.gov/eohhs/docs/dph/health-equity/clas-appendices-glossary.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix B: National CLAS Standards Enhancement Initiative 155
Appendix B: National CLAS Standards Enhancement Initiative
Background
In 2000, the Office of Minority Health at the U.S. Department of Health and Human Services published
the
National Standards for Culturally and Linguistically Appropriate Services in Health Care
, known as the
National CLAS Standards. The development process began in 1999, when the Office of Minority Health
convened key stakeholders to begin crafting a set of national standards that would guide the care
provided to the nation’s culturally and linguistically diverse populations. Published in 2000, the
National
Standards for Culturally and Linguistically Appropriate Services in Health Care: Final Report
resulted from
extensive research, discussions, and input from thousands of citizens. The original National CLAS
Standards provided a common understanding and guidance regarding cultural and linguistic competency,
with the ultimate goal of reducing racial and ethnic health disparities.
The original National CLAS Standards, the first of their kind, have served as catalyst and conduit for
efforts to improve quality of care and achieve health equity over the past 10 years. In recognition of
those vast changes, the Office of Minority Health undertook the National CLAS Standards Enhancement
Initiative from 2010 to 2012. Although much progress has been made toward universal implementation of
culturally and linguistically appropriate services, there is still much work to be done. The enhanced
National CLAS Standards seek to set a new bar for culturally and linguistically appropriate services to
improve the health of our ever-diversifying communities.
Goals
o To examine the National CLAS Standards, originally promulgated in 2000, for their relevance and
applicability to the 21
st
century
o To have the enhanced National CLAS Standards serve as the cornerstone for culturally and
linguistically appropriate services in the United States
o To launch new and innovative promotion and marketing initiatives for the National CLAS
Standards
o To coordinate the National CLAS Standards Enhancement Initiative with the Affordable Care Act
and other cultural and linguistic competency standards (e.g., The Joint Commission, National
Committee for Quality Assurance)
o To address the following areas throughout the enhancement initiative process:
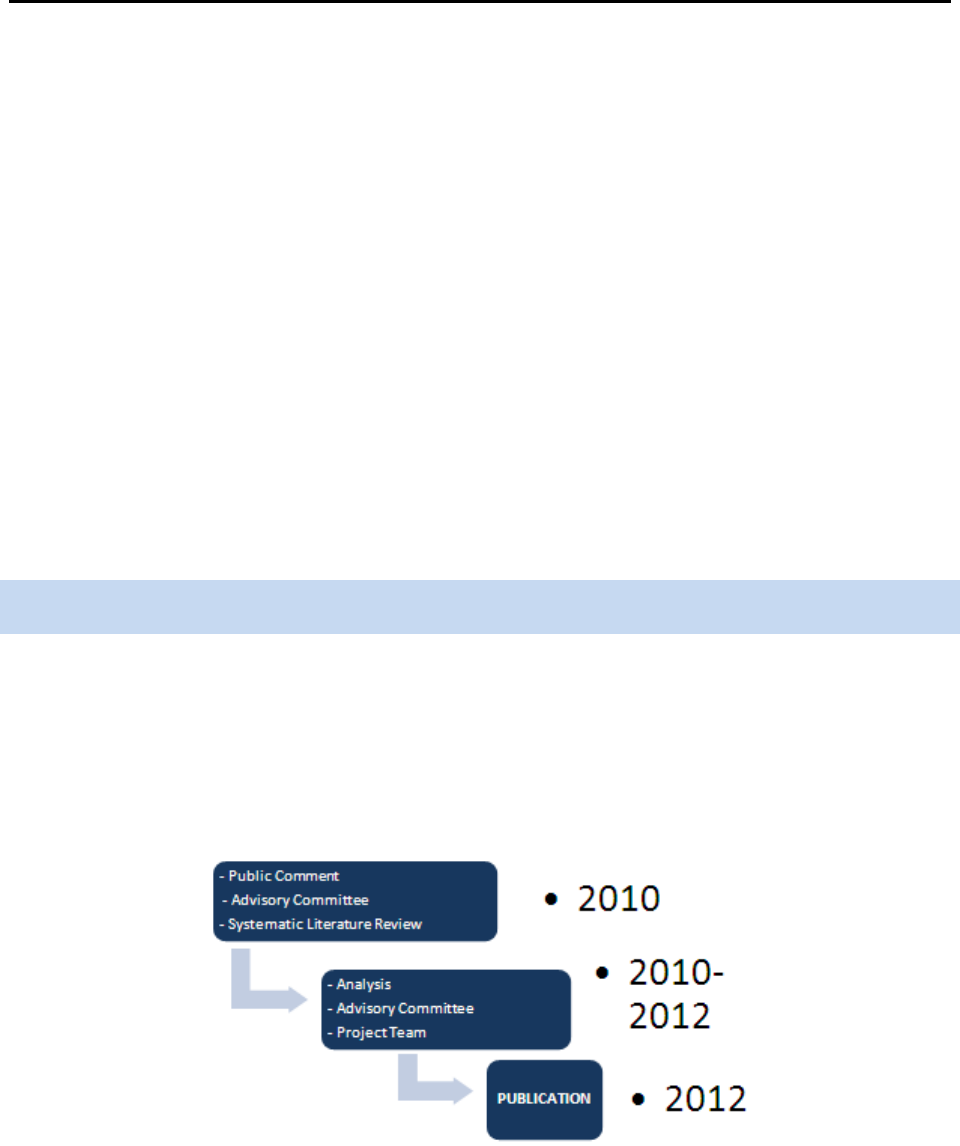
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix B: National CLAS Standards Enhancement Initiative 156
• Increase awareness regarding the importance and influence of cultural and linguistic
competency
• Increase impact of National CLAS Standards by expanding scope, audience, and
inclusivity
• Ensure the National CLAS Standards converge with the organization’s quality
improvement efforts
• Assist in the implementation of the Standards through additional resources
• Incorporate health literacy
• Promote the importance of research regarding the efficacy of the Standards
• Address advancements and developments in the field, including health care reform
o To promulgate an enhanced version of the National CLAS Standards
Development Process
Discussions began in 2009 at the HHS Office of Minority Health regarding a plan to enhance the National
CLAS Standards. The National CLAS Standards Enhancement Initiative formally began in 2010 following
the same development process as the original National CLAS Standards project in 1999–2001. The
development process had three major components: public comment, the Advisory Committee, and a
systematic literature review.
Figure 4: Phases of the National CLAS Standards Enhancement Initiative
o
Public Comment:
Three regional public meetings were held in fall 2010 in the same locations
as in the 2001 National CLAS Standards’ development: Baltimore, MD; Chicago, IL; and San
Francisco, CA. Public comment was also collected via written and online submissions during the
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix B: National CLAS Standards Enhancement Initiative 157
same time period. A public comment meeting report and a public comment online and written
submissions report are available online at www.ThinkCulturalHealth.hhs.gov.
o
National Project Advisory Committee:
A National Project Advisory Committee was convened
in 2010 and provided input and review throughout the development process, including several in-
person and virtual meetings. Members of the Advisory Committee represent the public, private,
and government sectors. It includes stakeholders representing a variety of health settings, such
as managed care, community health centers, insurance providers, local and state health
departments, community- and faith-based organizations, and federal government officials.
o
Systematic Literature Review:
A systematic literature review was developed in 2010 to use
as foundational knowledge for the Enhancement Initiative. This report provided a synthesis of
accomplishments, advances, and promising practices in the field since the publication of the
National CLAS Standards in 2000.
Public Comment
Public comment was collected in fall 2010 through meetings across the country, an online submission
portal, and written submissions. The announcement of the public comment opportunities appeared in the
Federal Register published on Sept. 23, 2010.
Public Comment Meetings
Three public comment meetings were held:
o Baltimore, MD; Oct. 22, 2010
o San Francisco, CA; Nov. 4, 2010
o Chicago, IL; Nov. 15, 2010
E
ach public comment meeting gathered detailed input from individuals and organizations. It included
open-microphone public comment and small group discussions with guided questions and group
feedback. The following themes arose from the comments heard across the three meetings.
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix B: National CLAS Standards Enhancement Initiative 158
The enhanced National CLAS Standards should:
o Encompass a broad definition of culture to include religion and spirituality; the lesbian, gay,
bisexual, and transgender community; deaf and hard of hearing individuals; and individuals with
limited vision
o Incorporate the areas of patient satisfaction and safety
o Address issues of health literacy
o Establish congruency with other standards in the field
o Be action oriented
o Reflect advancements in terminology, technology, and more, including medical homes, electronic
health records, and language access
Written and Online Public Comment
Written and online public comment was collected from Sept. 20, 2010, to Dec. 31, 2010. The following
overarching themes emerged:
The National CLAS Standards should:
o Expand the target audience beyond health care organizations
o Encompass a broad definition of culture to include religion and spirituality; the lesbian, gay,
bisexual, and transgender community; hard of hearing and deaf individuals; and individuals with
limited vision
o Offer more guidance within the Standards pertaining to language assistance services
o Establish congruency with other Standards in the field
National Project Advisory Committee
The National CLAS Standards Enhancement Initiative’s National Project Advisory Committee comprises 36
experts in the fields of cultural and linguistic competency representing HHS agencies, academic
institutions, health associations, and other not-for-profit organizations. The Advisory Committee provided
insight, recommendations, and review throughout the development of the enhanced Standards and the

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix B: National CLAS Standards Enhancement Initiative 159
Blueprint. The Enhancement Initiative Project Team
2
convened several meetings with the Advisory
Committee throughout the Enhancement Initiative, either in person or virtually (see Figure 5).
Figure 5: Advisory Committee Meetings
The Project Team conducted informal interviews in fall 2010 with the members of the Advisory
Committee in order to gather input on the National CLAS Standards from subject matter experts
representing a myriad of roles in the field of cultural and linguistic competency. These conversations,
along with the public comment and the systematic literature review, served to begin the laying of the
foundation for the enhanced National CLAS Standards in fall 2010. The topics of discussion included the
purpose and scope of the future National CLAS Standards, the target audience, and issues surrounding
implementation and promotion.
At the January 2011 meeting, the Advisory Committee discussed the following topics in depth:
2
The Enhancement Initiative Project Team was managed by an outside contractor. Team members are identified in Appendix C.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix B: National CLAS Standards Enhancement Initiative 160
o Purpose
o Definitions
o Inclusivity
o Audience
o Health Literacy
o Language Access Services
o Measurements
o Implementation
o Promotion
o End Product
The January 2011 meeting built the framework for the project team to begin drafting the enhanced
National CLAS Standards. During spring 2011, the Advisory Committee reviewed and provided feedback
on a document of terminology and definitions that would serve as the conceptual underpinning of the
enhanced National CLAS Standards. The Advisory Committee met virtually for a series of webinars in
summer 2011 to define the direction of the enhanced National CLAS Standards and discuss draft
Standards. In addition, the committee members began compiling information and materials for the
guidance document to accompany the enhanced National CLAS Standards.
The Advisory Committee provided in-depth reviews of the enhanced Standards’ drafts in late summer and
fall 2011. It also reviewed a draft of this guidance document to be published with the National CLAS
Standards. The Advisory Committee met in December 2011 to finalize the National CLAS Standards and
its report and make plans for the next steps.
Systematic Literature Review
The systematic literature review, developed in 2010, discusses the evolution of the efforts to improve
cultural and linguistic appropriateness since the release of the National CLAS Standards in 2000.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix B: Glossary 161
It addresses the broad dissemination, promotion, and implementation nationwide of the National CLAS
Standards and the concepts of CLAS. In addition, the report covers cultural competency education
initiatives; adoption of CLAS at the federal, state, and organizational levels; changes in accreditation
standards to explicitly include CLAS; the proliferation of technical assistance regarding CLAS; and
research and evaluation of the National CLAS Standards’ impact. The report concludes with areas for
consideration that emerged from the literature and research of the last 10 years, which provided insight
into the issues the enhanced National CLAS Standards should address.

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix C: National Project Advisory Committee 162
Appendix C: National Project Advisory Committee
Affiliations listed for identification purposes only; no endorsement of this report by Advisory Committee
members or their employers should be inferred.
Wilma Alvarado-Little, M.A., M.S.W.
Albany, New York
Chair of the Policy and Research Committee,
National Council on Interpreting in Health Care
Director of the Community Engagement/
Outreach Core, Center for the Elimination of
Minority Health Disparities at the University of
Albany,
State University of New York
Dennis Andrulis, Ph.D., M.P.H.
Austin, Texas
Associate Professor, University of Texas School
of Public Health
Senior Research Scientist, Texas Health Institute
Frances E. Ashe-Goins, R.N., M.P.H.
Washington, District of Columbia
Deputy Director
Office on Women’s Health
U.S. Department of Health and Human Services
George Askew, M.D.
Washington, District of Columbia
Chief Medical Officer
Administration for Children and Families
U.S. Department of Health and Human Services
Arlene Austin
Baltimore, Maryland
Director
Office of Equal Opportunity and Civil Rights
Centers for Medicare and Medicaid Services
U.S. Department of Health and Human Services
Charlene Avery, M.D.
Rockville, Maryland
Director
Office of Clinical and Preventive Services
Indian Health Service
U.S. Department of Health and Human Services
Lynne Bergero, M.H.S.A.
Oakbrook Terrace, Illinois
Project Director in the Division of Healthcare
Quality Evaluation, The Joint Commission
Cindy Brach, M.P.P.
Rockville, Maryland
Senior Health Policy Researcher
Agency for Healthcare Research and Quality
U.S. Department of Health and Human Services
Jessica Briefer French, M.H.S.A.
Washington, District of Columbia
Senior Consultant for Research, National
Committee for Quality Assurance
Jeffrey Caballero, M.P.H.
Oakland, California
Executive Director, Association of Asian Pacific
Community Health Organizations
Carol Crecy
Washington, District of Columbia
Aging Program Specialist
Administration for Community Living
U.S. Department of Health and Human Services
Linda Cummings, Ph.D.
Washington, District of Columbia
Vice President, National Association of Public
Hospitals and Health Systems
Director, The National Public Health and Hospital
Institute
Irene Dankwa-Mullan, M.D., M.P.H.
Bethesda, Maryland
Medical Officer
Division of Scientific Programs
National Institutes of Health
U.S. Department of Health and Human Services

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix C: National Project Advisory Committee 163
Kim Drumgo
Durham, North Carolina
Chief Diversity Official, Blue Cross Blue Shield of
North Carolina
Willarda V. Edwards, M.D., M.B.A.
Baltimore, Maryland
Past President, National Medical Association
Leonard Epstein, MSW
Rockville, Maryland
Senior Advisor
Clinical Quality and Culture
Health Resources and Services Administration
U.S. Department of Health and Human Services
Ron Finch, Ed.D.
Washington, District of Columbia
Vice President, National Business Group on
Health
Iris Garcia-Caban, Ph.D.
Quincy, Massachusetts
Performance Improvement Policy Analyst,
Massachusetts Executive Office of Health and
Human Services Medicaid Program
Rose Gonzalez, Ph.D., M.P.S., R.N.
Silver Spring, Maryland
Director of Government Affairs, American Nurses
Association
Tawara Goode, M.A.
Washington, District of Columbia
Assistant Professor & Director, National Center
for Cultural Competence, Georgetown University
Fred Hobby, M.A., CDM
Chicago, Illinois
President and CEO, Institute For Diversity in
Health Management of the American Hospital
Association
Roslyn Holliday Moore
Rockville, Maryland
Senior Advisor
Office of Behavioral Health Equity
Substance Abuse and Mental Health Services
Administration
U.S. Department of Health and Human Services
Sonja Hutchins, M.D., M.P.H., Dr. P.H.
Atlanta, Georgia
Senior Medical Epidemiologist
Office of Minority Health and Health Equity
Centers for Disease Control and Prevention
U.S. Department of Health and Human Services
Thomas LaVeist, Ph.D.
Baltimore, Maryland
Director, Center for Health Disparities Solutions,
Johns Hopkins University
Heather R. Lawson, J.D., M.P.H.
Washington, District of Columbia
Civil Rights Analyst
Office for Civil Rights
U.S. Department of Health and Human Services
Robert C. Like, M.D., M.S.
New Brunswick, New Jersey
Professor and Director, Center for Healthy
Families and Cultural Diversity, Department of
Family Medicine and Community Health,
University of Medicine and Dentistry of New
Jersey – Robert Wood Johnson Medical School
Francis G. Lu, M.D.
Sacramento, California
Luke & Grace Kim Professor in Cultural
Psychiatry and Director of Cultural Psychiatry,
Department of Psychiatry & Behavioral Sciences,
University of California, Davis
Luben Montoya, J.D., M.P.A.
Washington, D.C.
Supervisory Civil Rights Analyst
Office for Civil Rights
U.S. Department of Health and Human Services
Carmen Nevarez, M.D., M.P.H.
Oakland, California
Vice President of External Relations and
Preventive Medicine Advisor, Public Health
Institute
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix C: National Project Advisory Committee 164
Guadalupe Pacheco, M.S.W.
Rockville, Maryland
Senior Health Advisor to the Director
Office of Minority Health
U.S. Department of Health and Human Services
Elena Rios, M.D., M.S.P.H.
Washington, District of Columbia
President & CEO, National Hispanic Medical
Association
Susan Matsuko Shinagawa
Spring Valley, California
Co-Founder & Past Chair, Asian and Pacific
Islander National Cancer Survivors Network,
Asian & Pacific Islander American Health Forum
Past Chair, Intercultural Cancer Council
Lisa Strumwasser
Washington, District of Columbia
Special Assistant
Office of the Assistant Secretary for Legislation
U.S. Department of Health and Human Services
Ileen Sylvester, M.B.A.
Anchorage, Alaska
Vice President of Executive and Tribal Services,
Southcentral Foundation
Gayle Tang, M.S.N., R.N.
Oakland, California
Senior Director, National Linguistic and Diversity
Infrastructure Management
Kaiser Permanente, National Diversity
Ho Tran, M.D., M.P.H.
San Francisco, California
President and CEO, National Council of Asian
and Pacific Islander Physicians
Matthew K. Wynia, M.D., M.P.H., FACP
Chicago, Illinois
Director of The Institute for Ethics and The
Center for Patient Safety, American Medical
Association
Mara Youdelman, J.D., LLM
Washington, District of Columbia
Chair, Certificate Commission for Healthcare
Interpreters
Senior Attorney, National Health Law Program
Enhancement Initiative Project Team
C. Godfrey Jacobs
Project Manager
SRA International, Inc.
Darci L. Graves, M.P.P., M.A., M.A.
Senior Health Education & Policy Specialist
SRA International, Inc.
Jennifer Kenyon
Senior Research Associate
SRA International, Inc.
Crystal L. Barksdale, Ph.D.
Senior Research Analyst
SRA International, Inc.
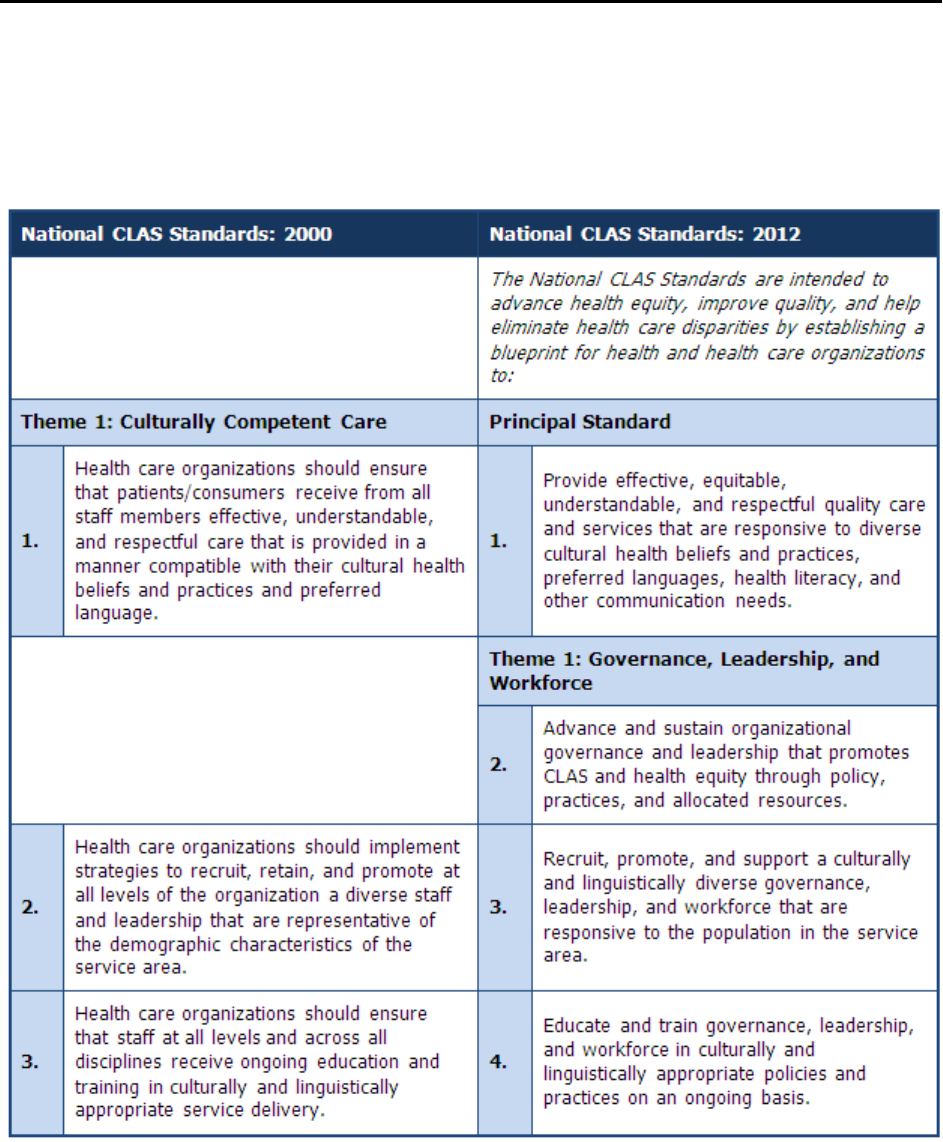
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix D: Crosswalk – National CLAS Standards 2000 and 2012 165
Appendix D: Crosswalk – National CLAS Standards 2000 and 2012
National Standards for Culturally and Linguistically Appropriate Services (CLAS) in Health
and Health Care
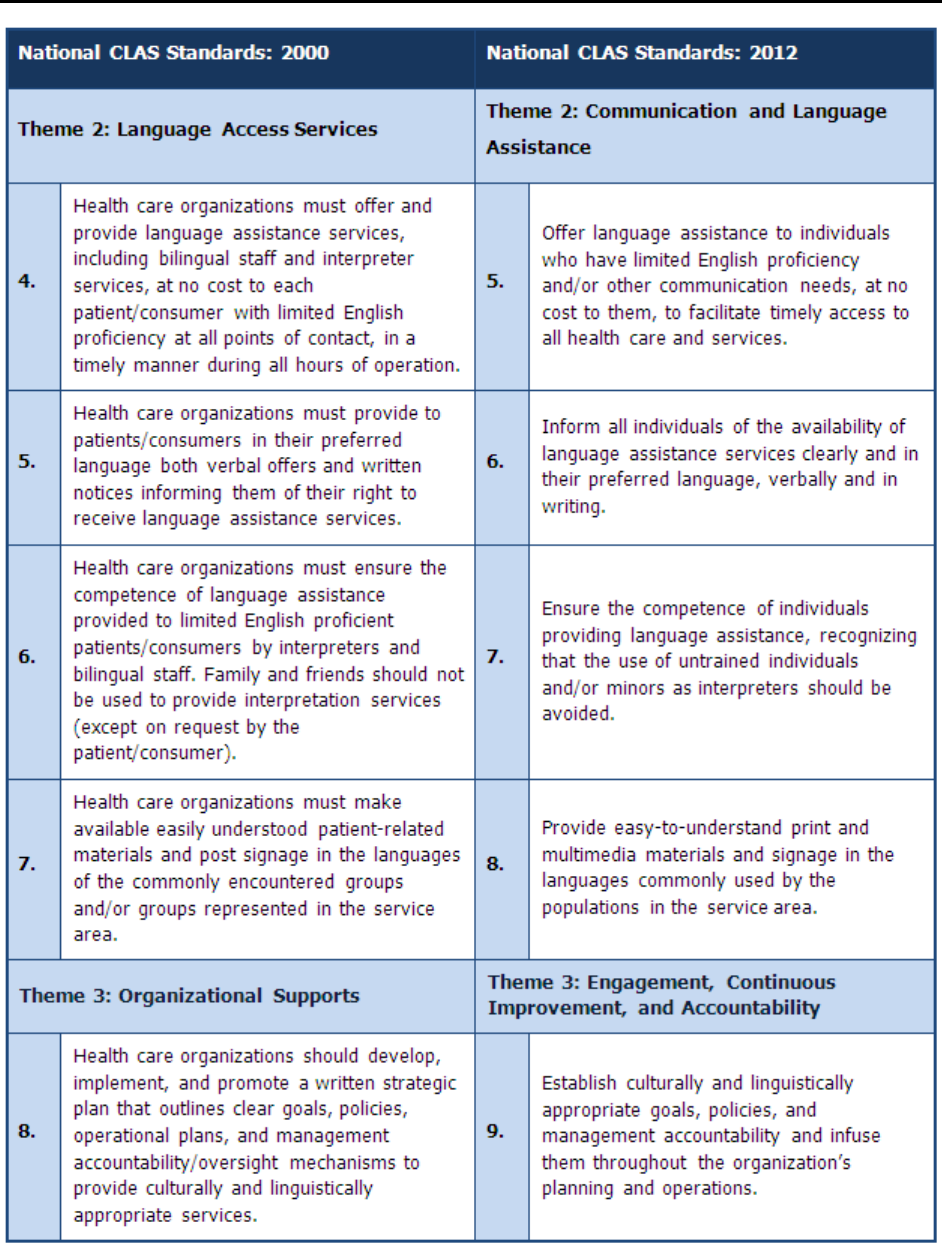
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix D: Crosswalk – National CLAS Standards 2000 and 2012 166

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix D: Crosswalk – National CLAS Standards 2000 and 2012 167
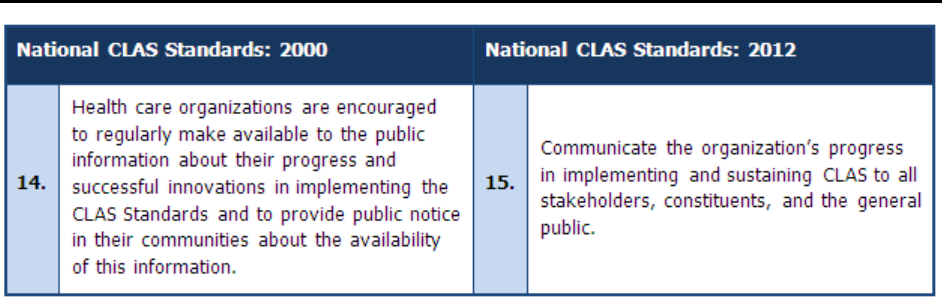
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix D: Crosswalk – National CLAS Standards 2000 and 2012 168
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 169
Appendix E: Resources
Appendix E provides an expanded list of resources, organized by the National CLAS Standards’ themes,
that pertain to advancing and sustaining CLAS policy and practice. The table below provides an overview
of the Standards and the themes in which they are found.
Theme Standards
Principal Standard
o Provide effective, equitable, understandable, respectful, and quality
care and services that are responsive to diverse cultural health beliefs
and practices, preferred languages, health literacy, and other
communication needs.
Theme 1:
Governance, Leadership,
and Workforce
o Advance and sustain governance and leadership that promotes CLAS
and health equity
o Recruit, promote, and support a diverse governance, leadership, and
workforce
o Educate and train governance, leadership, and workforce in CLAS
Theme 2:
Communication and
Language Assistance
o Offer communication and language assistance
o Inform individuals of the availability of language assistance
o Ensure the competence of individuals providing language assistance
o Provide easy-to-understand materials and signage
Theme 3:
Engagement,
Continuous
Improvement, and
Accountability
o Infuse CLAS throughout the organization’s planning and operations
o Conduct organizational assessments
o Collect and maintain demographic data
o Conduct assessments of community health assets and needs
o Partner with the community
o Create conflict and grievance resolution processes
o Communicate the organization’s progress regarding CLAS
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 170
Principal Standard Resources
Adelman, L. (Creator, Producer). (2008).
Unnatural causes: Is inequality making us sick?
[Documentary
series]. United States: California Newsreel with Vital Pictures.
Advisory Commission on Consumer Protection and Quality in the Health Care Industry. (1997).
Consumer
bill of rights and responsibilities: Report to the President of the United States.
Retrieved from
http://www.opm.gov/insure/archive/health/cbrr.htm
American Association on Intellectual and Developmental Disabilities. (n.d.).
Definition of intellectual
disability.
Retrieved from http://www.aaidd.org/content_100.cfm?navID=21
American Medical Association. (2006). Content area 4. Develop workforce. In
Improving communication,
improving care: How health care organizations can ensure effective, patient-centered communication
with people from diverse populations
(pp. 47–54). Retrieved from http://www.ama-
assn.org/resources/doc/ethics/pcc-consensus-report.pdf
American Medical Association. (2006). Content area 5a. Socio-cultural context. In
Improving
communication, improving care: How health care organizations can ensure effective, patient-centered
communication with people from diverse populations
(pp. 61–65). Retrieved from http://www.ama-
assn.org/resources/doc/ethics/pcc-consensus-report.pdf
Beach, M. C., Saha, S., & Cooper, L. A. (2006).
The role and relationship of cultural competence and
patient-centeredness in health care quality.
Retrieved from The Commonwealth Fund website:
http://www.commonwealthfund.org/~/media/Files/Publications/Fund%20Report/2006/Oct/The%20Role
%20and%20Relationship%20of%20Cultural%20Competence%20and%20Patient%20Centeredness%20i
n%20Health%20Care%20Quality/Beach_rolerelationshipcultcomppatient%20cent_960%20pdf.pdf
Bobal, A. M., Brown, H. L., Hartman, T. L., Magee, M., & Schmidt, C. M. (2007). Navigating the US health
care system: A video guide for immigrant and diverse patient populations.
Journal of the Medical Library
Association, 95
(3), 286–289. doi:10.3163/1536-5050.95.3.286
Brach C., Keller, D, Hernandez, L., Baur, C., Parker, R., Schyve, P., Lemerise, & Schillinger, D. (2012).
Ten Attributes of Health Literate Health Care Organizations. Washington DC. Retrieved from:
http://www.iom.edu/Activities/PublicHealth/HealthLiteracy.aspx
Briefer French, J., Schiff, D., Han, E., & Weinick, R. (2008).
Multicultural health care: A quality
improvement guide.
Retrieved from National Committee for Quality Assurance website:
http://www.ncqa.org/portals/0/hedisqm/clas/clas_toolkit.pdf
California Pan-Ethnic Health Network. (2010).
Building quality & equitable health care systems.
(Conference report). Retrieved from
http://www.cpehn.org/pdfs/Building%20Quality%20and%20Equitable%20Health%20Care%20Systems
%2010-10.pdf
DeafMD.org.
(2012). Retrieved from http://www.deafmd.org
DiversityRx.
(2012). Retrieved from http://www.diversityrx.org/
EthnoMed.
(2012). Retrieved from http://ethnomed.org/
Frampton, S., Guastello, S., Brady, C., Hale, M., Smith, S. B., & Stone, S. (n.d.).
Patient-centered care:
Improvement guide.
Retrieved from http://www.patient-centeredcare.org/index.html
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 171
Principal Standard Resources
Galanti, G. A. (2008).
Caring for patients from different cultures: Case studies from American hospitals
(4th ed.). Philadelphia, PA: University of Pennsylvania Press.
Gallaudet University, Laurent Clerc National Deaf Education Center. (2008).
Healthcare for deaf and hard
of hearing patients: Clinics and special services.
Retrieved from
http://www.gallaudet.edu/clerc_center/information_and_resources/info_to_go/educate_children_(3_to_2
1)/social-
emotional_development/mental_health_and_wellness/hlthcare_delivery_for_dhoh_patients_clinicsspec_s
vcs.html
Gay and Lesbian Medical Association. (2001).
Healthy people 2010 companion document for lesbian, gay,
bisexual and transgender (LGBT) health.
Retrieved from
http://www.nalgap.org/PDF/Resources/HP2010CDLGBTHealth.pdf
Gay and Lesbian Medical Association.
(n.d.). Retrieved from http://www.glma.org/
The George Washington Institute for Spirituality and Health.
(n.d.). Retrieved from
http://www.gwish.org/
Goldney, R. D., Fisher, L. I., & Wilson, D. H. (2001). Mental health literacy: An impediment to the
optimum treatment of major depression in the community.
Journal of Affective Disorders, 64
(2–3), 277–
84.
Harmer, L. (1999). Health care delivery and deaf people: Practice, problems, and recommendations for
change.
Journal of Deaf Studies and Deaf Education, 4
(2), 73–110. doi:10.1093/deafed/4.2.73
Health Research & Educational Trust, Institute for Diversity in Health Management (2011).
Building a
culturally competent organization: The quest for equity in health care.
Retrieved from
http://www.hret.org/quality/projects/resources/cultural-competency.pdf
HealthCare Chaplaincy. (2009).
Cultural and spiritual sensitivity: A learning module for health care
professionals.
Retrieved from http://www.healthcarechaplaincy.org/userimages/A Dictionary of Patients'
Spiritual Cultural Values for Health Care Professionals_ July 2011.pdf
HealthCare Chaplaincy. (2011).
A dictionary of patients’ spiritual & cultural values for health care
professionals.
Retrieved from http://www.healthcarechaplaincy.org/userimages/doc/A-Dictionary-of-
Patients'-Spiritual-Cultural-Values-for-Health-Care-Professionals.pdf
Hearing Loss Association of America.
(2012). Retrieved from http://www.hearingloss.org/
Herndon, J., Chaney, M., & Carden, D. (2011). Health literacy and emergency department outcomes: A
systematic review.
Annals of Emergency Medicine, 57
(4), 334–345.
doi:10.1016/j.annemergmed.2010.08.035.
Institute for Patient- and Family-Centered Care.
(2012). Retrieved from http://www.ipfcc.org
Institute of Medicine, Committee on Future Directions for the National Healthcare Quality and Disparities
Reports. (2010).
Future directions for the national healthcare quality and disparities reports.
Retrieved
from http://www.ahrq.gov/research/iomqrdrreport/iomqrdrreport.pdf
International Medical Interpreters Association. (2012).
National interpreter advocacy forum.
Retrieved
from http://www.imiaweb.org/advocacy/NatIntAdvForum.asp
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 172
Principal Standard Resources
International Society for Urban Health.
(2005). Retrieved from http://www.isuh.org/
Johns Hopkins Medicine. (n.d.).
Diversity & inclusion 2020.
Retrieved from
http://www.hopkinsmedicine.org/bin/s/x/diversity_and_inclusion.pdf
Johns Hopkins Medicine. (n.d.).
Diversity and inclusion at Johns Hopkins: Commitment, passion,
engagement.
Retrieved from http://www.hopkinsmedicine.org/diversity/index.html
Johns Hopkins University. (2012).
Johns Hopkins Urban Health Institute.
Retrieved from
http://urbanhealth.jhu.edu/
The Joint Commission. (2010). Patient communication assessment tool [Figure 5-1]. In
Advancing
effective communication, cultural competence, and patient- and family-centered care: A roadmap for
hospitals.
Retrieved from
http://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf
The Joint Commission. (2011).
Advancing effective communication, cultural competence, and patient-
and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field
guide.
Retrieved from http://www.jointcommission.org/assets/1/18/LGBTFieldGuide.pdf
Journal of Multicultural Counseling and Development.
(2012). Retrieved from http://www.jmcdonline.org/
Journal of Religion and Health.
(n.d.). Retrieved from
http://www.springer.com/public+health/journal/10943
Institute of Medicine, Committee on Understanding and Eliminating Racial and Ethnic Disparities in
Health Care, Board on Health Sciences Policy. (2003). B. D. Smedley, A. Y. Stith, & A. R. Nelson (Eds.).
Unequal treatment: Confronting racial and ethnic disparities in health care.
Retrieved from
http://www.nap.edu/openbook.php?record_id=10260&page=R1
Kleinman, A. (1981).
Patients and healers in the context of culture: An exploration of the borderland
between anthropology, medicine, and psychiatry.
Berkeley, CA: University of California Press.
Kline, M. V. (1999). Planning health promotion and disease prevention programs in multicultural
populations. In R. M. Huff & M. V. Kline (Eds.),
Promoting health in multicultural populations: A
handbook for practitioners
(pp. 73–102). Thousand Oaks, CA: SAGE Publications, Inc.
Kutob, R. M., Senf, J. H., & Harris, J. M. (2009). Teaching culturally effective diabetes care: Results of a
randomized controlled trial.
Family Medicine, 41
(3), 167–174. Retrieved from
http://www.stfm.org/fmhub/fm2009/March/Randa167.pdf
Lighthouse International.
(n.d.). Retrieved from http://www.lighthouse.org
Massachusetts Department of Public Health, Office of Health Equity. (2009).
Making CLAS happen: Six
areas for action.
Retrieved from http://www.mass.gov/eohhs/provider/guidelines-resources/services-
planning/workforce-development/health-equity/clas/making-clas-happen.html
Massachusetts General Hospital, The Committee on Racial and Ethnic Disparities. (n.d.).
Subcommittees.
Retrieved from http://www.mghdisparities.org/sub_quality.html
Meade, C., Menard, J., Martinez, D., & Calvo, A. (2007). Impacting health disparities through community
outreach: Utilizing the CLEAN look (culture, literacy, education, assessment, and networking).
Cancer
Control, 14
(1), 70–77. Retrieved from http://www.moffitt.org/CCJRoot/v14n1/pdf/70.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 173
Principal Standard Resources
MedlinePlus. (2012).
Rural health concerns.
Retrieved from
http://www.nlm.nih.gov/medlineplus/ruralhealthconcerns.html
National Coalition for LGBT Health.
(n.d.). Retrieved from http://lgbthealth.webolutionary.com/
National Committee for Quality Assurance. (2009).
Implementing multicultural health care standards:
Ideas and examples.
Retrieved from
http://www.ncqa.org/Portals/0/Publications/Implementing%20MHC%20Standards%20Ideas%20and%20
Examples%2004%2029%2010.pdf
National Committee for Quality Assurance. (2011).
Awards: Recognizing innovations in multicultural
health care.
Retrieved from http://www.ncqa.org/tabid/453/Default.aspx
National Council on Interpreting in Health Care.
(2011). Retrieved from http://www.ncihc.org
National Health Law Program.
(2010). Retrieved from http://www.healthlaw.org/
National Health Plan Collaborative. (2008).
The national health plan collaborative toolkit.
Retrieved from
Robert Wood Johnson Foundation website: http://www.rwjf.org/qualityequality/product.jsp?id=33960
National Partnership for Action to End Health Disparities. (2011).
National stakeholder strategy for
achieving health equity.
Retrieved from U.S. Department of Health and Human Services, Office of
Minority Health website:
http://www.minorityhealth.hhs.gov/npa/templates/content.aspx?lvl=1&lvlid=33&ID=286
National Patient Safety Foundation. (n.d.).
Ask me 3.
Retrieved from http://www.npsf.org/for-healthcare-
professionals/programs/ask-me-3
National Quality Forum. (2005).
Implementing a national voluntary consensus standard for informed
consent: A user’s guide for healthcare professionals.
Retrieved from
http://www.qualityforum.org/Publications/2005/09/Implementing_a_National_Voluntary_Consensus_Stan
dard_for_Informed_Consent__A_User%e2%80%99s_Guide_for_Healthcare_Professionals.aspx
National Quality Forum. (2005).
Improving patient safety through informed consent for patients with
limited health literacy.
Retrieved from
http://www.qualityforum.org/Publications/2005/09/Improving_Patient_Safety_Through_Informed_Conse
nt_for_Patients_with_Limited_Health_Literacy.aspx
National Quality Forum. (2009).
A comprehensive framework and preferred practices for measuring and
reporting cultural competency: A consensus report.
Retrieved from
http://www.cpehn.org/pdfs/Cultural%20Competency%20-%20NQF.pdf
National Rural Health Association.
(2012). Retrieved from http://www.ruralhealthweb.org/
National Rural Health Association. (2012).
Rural Multiracial and Multicultural Health Conference.
http://www.ruralhealthweb.org/go/events/rural-multiracial-and-multicultural-health-conference
New York State Office of Mental Health Office of Quality Management. (2011).
Quality improvement plan
template.
Retrieved from http://omh.ny.gov/omhweb/cqi/plan_template.html
Papps, E., & Ramsden, I. (1996). Cultural safety in nursing: The New Zealand experience.
International
Journal for Quality in Health Care, 8
(5), 491–497. doi:10.1093/intqh/8.5.491
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 174
Principal Standard Resources
Patak, L., Wilson-Stronks, A., Costello, J., Kleinpell, R., Henneman, E., Person, C., & Happ, M. B. (2009).
Improving patient-provider communication: A call to action.
Journal of Nursing Administration, 39
(9),
372–376. doi:10.1097/NNA.0b013e3181b414ca
Pfizer. (2011).
Prevalence calculator.
Retrieved from http://www.pfizerhealthliteracy.com/physicians-
providers/PrevalenceCalculator.aspx
Putsch, R., SenGupta, I., Sampson, A., & Tervalon, M. (2003).
Reflections on the CLAS Standards: Best
practices, innovations and horizons.
Retrieved from The Cross Cultural Health Care Program website:
http://www.xculture.org/files/CLAS.Standards.Report.pdf.pdf
QSource, Underserved Quality Improvement Organization Support Center. (2005).
CLAS Standards
implementation tips.
Retrieved from
http://www.qsource.org/uqiosc/CLAS%20Standards%20Strategies%5B7AUG-2005%5D.pdf
Refugee Health Technical Assistance Center.
(2011). Retrieved from http://www.refugeehealthta.org/
Robert Wood Johnson Foundation. (2008).
Speaking together toolkit.
Retrieved from
http://www.rwjf.org/pr/product.jsp?id=29653
Saha, S., Beach, M. C., & Cooper, L. A. (2008). Patient centeredness, cultural competence and healthcare
quality.
Journal of the National Medical Association, 100
(11), 1275–1285. Retrieved from
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2824588
Salimbene, S. (2001).
CLAS A–Z: A practical guide for implementing the National Standards for Culturally
and Linguistically Appropriate Services (CLAS) in health care.
Retrieved from Office of Minority Health
website: http://minorityhealth.hhs.gov/assets/pdf/checked/CLAS_a2z.pdf
Savinar, R. (n.d.).
California take on “promotora” model of community outreach a success.
Retrieved
from Proyecto Vision website: http://www.proyectovision.net/english/news/13/promotoras.html
Smith, W., Betancourt, J., Wynia, M., Bussey-Jones J., Stone, V., Phillips, C., … & Bowles, J. (2007).
Recommendations for teaching about racial and ethnic disparities in health and health care.
Annals of
Internal Medicine, 147
(9), 654–665.
Spector, R. E. (2008).
Cultural diversity in health & illness
(7th ed.). Upper Saddle River, NJ: Pearson
Prentice Hall.
Spiritual Diversity and Social Work Resource Center.
(n.d.). Retrieved from
http://www.socwel.ku.edu/candagrant/hfc4.htm
State Govern
ment of Victoria, Australia, Department of Health, Rural and Regional Health and Aged Care
Services. (2009).
Cultural responsiveness framework: Guidelines for Victorian health services.
Retrieved
from http://www.health.vic.gov.au/__data/assets/pdf_file/0008/381068/cultural_responsiveness.pdf
Stonecypher, K. (2009). Creating a patient education tool.
Journal of Continuing Education in Nursing,
40
(10), 462–467. doi:10.3928/00220124-20090923-06
Tanenbaum Center for Interreligious Understanding. (2009).
The medical manual for religio-cultural
competence: Caring for religiously diverse populations.
New York, NY: Tanenbaum Center for
Interreligious Understanding.
Transcultural Nursing Society.
(2012). Retrieved from http://www.tcns.org/
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 175
Principal Standard Resources
University of California, San Francisco. (2008).
LGBT resource center.
Retrieved from
http://lgbt.ucsf.edu/services_health.html
University of Illinois at Urbana-Champaign, McKinley Health Center. (2009).
Multicultural health
clearinghouse.
Retrieved from http://www.mckinley.illinois.edu/multiculturalhealth/index.htm
University of Rochester Medical Center. (2012).
National Center for Deaf Health Research.
Retrieved from
http://www.urmc.rochester.edu/ncdhr/
U.S. Department of Commerce, Census Bureau. (2004).
2004 U.S. Census test: Language identification
flashcard.
Retrieved from http://www.lep.gov/ISpeakCards2004.pdf
U.S. Department of Health and Human Services. (2011).
HHS action plan to reduce racial and ethnic
health disparities: A nation free of disparities in health and health care.
Retrieved from
http://minorityhealth.hhs.gov/npa/files/Plans/HHS/HHS_Plan_complete.pdf
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2010).
Developing quality of care measures for people with disabilities: Summary of expert meeting
(AHRQ
Publication No. 10-0103)
.
Retrieved from http://www.ahrq.gov/populations/devqmdis/devqmdis.pdf
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2010).
Health literacy universal precautions toolkit
(AHRQ Publication No. 10-0046-EF). Retrieved from
http://www.ahrq.gov/qual/literacy/
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2011).
2010 national healthcare disparities report
(AHRQ Publication No. 11-0005). Retrieved from
http://www.ahrq.gov/qual/nhdr10/nhdr10.pdf
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2011).
CAHPS cultural competence item set.
Retrieved from https://www.cahps.ahrq.gov/surveys-
guidance/item-sets/cultural-competence.aspx
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2011).
Ensuring that patient centered medical homes effectively serve patients with complex needs
(AHRQ
Publication No. 11-0109)
.
Retrieved from
http://pcmh.ahrq.gov/portal/server.pt/community/pcmh__home/1483/pcmh_tools___resources_patient-
centered_v2
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2012).
Coordinating care for adults with complex care needs in the patient-centered medical home: Challenges
and solutions
(AHRQ Publication No. 12-0010)
.
Retrieved from
http://pcmh.ahrq.gov/portal/server.pt/community/pcmh__home/1483/pcmh_tools___resources_coordina
ted_care_v2
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2012).
AHRQ Healthcare Innovations Exchange: Innovations and tools to improve quality and reduce disparities.
Retrieved from http://www.innovations.ahrq.gov/
U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. (n.d.)
Intellectual disability fact sheet.
Retrieved from
http://www.cdc.gov/ncbddd/actearly/pdf/parents_pdfs/IntellectualDisability.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 176
Principal Standard Resources
U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. (2011).
Lesbian, gay, bisexual and transgender health.
Retrieved from http://www.cdc.gov/lgbthealth
U.S. Department of Health and Human Services, Office for Civil Rights. (2003).
Guidance to federal
financial assistance recipients regarding Title VI and the prohibition against national origin discrimination
affecting limited English proficient persons.
Retrieved from
http://www.hhs.gov/ocr/civilrights/resources/laws/revisedlep.html
U.S. Department of Health and Human Services, Office of Minority Health. (2011).
National Partnership
for Action to End Health Disparities.
Retrieved from http://minorityhealth.hhs.gov/npa
U.S. Department of Health and Human Services, Office of Minority Health. (n.d.).
Think cultural health:
Advancing health equity at every point of contact.
Retrieved from
https://www.thinkculturalhealth.hhs.gov
U.S. Department of Health and Human Services, Specialized Information Services. (2012).
Outreach
activities and resources: Multi-cultural resources for health information.
Retrieved from
http://sis.nlm.nih.gov/outreach/multicultural.html
U.S. Department of Health and Human Services, Administration on Aging. (2010).
A toolkit for serving
diverse communities.
Retrieved from
http://www.aoa.gov/AOARoot/AoA_Programs/Tools_Resources/DOCS/AoA_DiversityToolkit_Full.pdf
Wilson-Stronks, A., & Galvez, E. (2007).
Hospitals, language, and culture: A snapshot of the nation.
Retrieved from The Joint Commission website: http://www.jointcommission.org/assets/1/6/hlc_paper.pdf
Wu, E., & Martinez, M. (2006).
Taking cultural competency from theory to action
(Commonwealth Fund
Publication No. 964). Retrieved from The Commonwealth Fund website:
http://www.commonwealthfund.org/usr_doc/Wu_takingcultcomptheoryaction_964.pdf
Wynia, M., & Matiasek, J. (2006).
Promising practices for patient-centered communication with
vulnerable populations: Examples from eight hospitals
(Commonwealth Fund Publication No. 947).
Retrieved from The Commonwealth Fund website:
http://www.commonwealthfund.org/~/media/Files/Publications/Fund%20Report/2006/Aug/Promising%2
0Practices%20for%20Patient%20Centered%20Communication%20with%20Vulnerable%20Populations%
20%20Examples%20from%20Ei/Wynia_promisingpracticespatientcentered_947%20pdf.pdf
Youdelman, M., & Perkins, J. (2005). Promising practices for small health care providers. In
Providing
language services in small health care provider settings: Examples from the field
(pp. 3–11)
(Commonwealth Fund Publication No. 810). Retrieved from The Commonwealth Fund website:
http://www.commonwealthfund.org/usr_doc/810_Youdelman_providing_language_services.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 177
Theme 1 Resources
Accreditation Council for Graduate Medical Education. (2011).
Common program requirements.
Retrieved
from http://www.acgme.org/acwebsite/home/common_program_requirements_07012011.pdf
American Academy of Family Physicians. (2001).
Quality care for diverse populations videos
[Video
series]. Available from http://www.aafp.org/online/en/home/clinical/publichealth/culturalprof/quality-
care-diverse-populations.html
American Academy on Communication in Healthcare. (n.d.).
Skills based courses
[Course summaries].
Retrieved from http://www.aachonline.org/?page=SkillsBasedCourses
American Medical Association, The Ethical Force Program. (2006). Content area 4. Develop workforce. In
Improving communication—improving care: How health care organizations can ensure effective, patient-
centered communication with people from diverse populations
(pp. 47–54). Retrieved from
http://www.ama-assn.org/resources/doc/ethics/pcc-consensus-report.pdf
American Medical Association. (2012).
C-CAT: Patient centered communication.
Retrieved from
http://www.ama-assn.org/go/ccat
American Medical Association. (2012).
The Ethical Force Program.
Retrieved from http://www.ama-
assn.org/ama/pub/physician-resources/medical-ethics/the-ethical-force-program.page
Archer, D. (Producer), & Silver, J. (Director). (1997).
A world of differences: Understanding cross-
cultural
communication
[DVD]. United States: University of California Extension Center for Media and
Independent Learning.
Association of American Medical Colleges (n.d.).
Tool for assessing cultural competence training (TACCT).
Retrieved from https://www.aamc.org/initiatives/tacct/
Beach, M. C., Price, E. G., Gary, T. L., Robinson, K. A., Gozu, A., Palacio, A., … Cooper, L. A. (2005).
Cultural competence: A systematic review of health care provider educational interventions.
Medical
Care, 43
(4), 356–373.
Betancourt, J. R. (2003). Cross-cultural medical education: Conceptual approaches and frameworks for
evaluation.
Academic Medicine, 78
(6), 560–569.
Betancourt, J., Green, A., & King, R. (2008).
Improving quality and achieving equity: A guide for hospital
leaders.
Retrieved from Massachusetts General Hospital, The Disparities Solutions Center website:
http://www2.massgeneral.org/disparitiessolutions/z_files/disparities%20leadership%20guide_final.pdf
Carter-Pokras, O., Acosta, D. A., Lie, D., Bereknyei, S., DeLisser, H., Haidet, P., … Glick, S. (2009).
Practice what you teach: Curricular products from the National Consortium for Multicultural Education for
Health Professionals.
Retrieved from
http://culturalmeded.stanford.edu/pdf%20docs/Focus%20MDNG%20NCME%20curricular%20products.p
df
Cross Cultural Health Care Program. (n.d.).
Course information: Bridging the gap
[Online training course
summary]. Retrieved from http://www.xculture.org/BTGclassdesc.php
Echeverri, M., Brookover, C., & Kennedy, K. (2010). Nine constructs of cultural competence for
curriculum development.
American Journal of Pharmaceutical Education, 74
(10), Article 181. Retrieved
from http://www.ajpe.org/doi/pdf/10.5688/aj7410181
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 178
Theme 1 Resources
Georgetown University Child Development Center, Center for Child Health and Mental Health Policy,
National Center for Cultural Competence. (2000).
A planner's guide: Infusing principles, content and
themes related to cultural and linguistic competence into meetings and conferences.
Retrieved from
http://gucchd.georgetown.edu/products/PlannersGuide.pdf
Gilbert, M. J. (Ed.). (2003).
A manager's guide to cultural competence education for health care
professionals.
Retrieved from The California Endowment website:
http://www.calendow.org/uploadedFiles/managers_guide_cultural_competence(1).pdf
Gilbert, M. J. (Ed.). (2003).
Principles and recommended standards for cultural competence education of
health care professionals.
Retrieved from The California Endowment website:
http://www.calendow.org/uploadedFiles/principles_standards_cultural_competence.pdf
Gilbert, M. J. (Ed.). (2003).
Resources in cultural competence education for health care professionals.
Retrieved from The California Endowment website:
http://www.calendow.org/uploadedFiles/resources_in_cultural_competence.pdf
Grainger-Monsen, M., & Haslett, J. (2004).
Worlds apart: A four-part series on cross-cultural healthcare
[Film series]. Fanlight Productions. Retrieved from The Commonwealth Fund website:
http://www.commonwealthfund.org/Multimedia/Videos/2004/Feb/Worlds-Apart---em--A-Film-Series-on-
Cross-Cultural-Health-Care.aspx
Graves, D. L., Like, R. C., Kelly, N., & Hohensee, A. (2007). Legislation as intervention: A survey of
cultural competence policy in health care.
Journal of Health Care Law and Policy, 10
(2), 339–361.
Retrieved from http://thecqc.org/uploads/Graves_et_al.pdf
Hark, A. L., & DeLisser, H. M. (Eds.). (2009).
Achieving cultural competency: A case-based approach to
training health professionals.
Oxford, UK: Wiley-Blackwell.
Institute for Diversity in Health Management. (2004).
Strategies for leadership: Does your hospital reflect
the community it serves? Diversity and cultural proficiency assessment tool for leaders.
Retrieved from
http://www.aha.org/content/00-10/diversitytool.pdf
Institute for Diversity in Health Management. (2008).
Institute Resource Center.
Retrieved from
http://www.diversityconnection.org/diversityconnection/membership/Institute-Resource-
Center.jsp?fll=S12
Institute for Healthcare Communication. (2012).
Training.
Retrieved from
http://healthcarecomm.org/training
Khanna, S. K., Cheyney, M., & Engle, M. (2009). Cultural competency in health care: Evaluating the
outcomes of a cultural competency training among health care professionals.
Journal of National Medical
Association, 101,
886–892.
Kripalani, S., & Jacobson, K. L. (2007).
Strategies to improve communication between pharmacy staff
and patients: Training program for pharmacy staff
[Curriculum guide] (AHRQ Publication No. 07(08)-
0051-1-EF). Retrieved from http://www.ahrq.gov/qual/pharmlit/pharmtrain.htm
Liaison Committee on Medical Education. (2011).
Functions and structure of a medical school: standards
for accreditation of medical education programs leading to the M.D. degree. IS-16, ED-21, ED-22.
Retrieved from http://www.lcme.org/functions2011may.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 179
Theme 1 Resources
Lie, D., Boker, J., & Cleveland, E. (2006). Using the tool for assessing cultural competence training
(TACCT) to measure faculty and medical student perceptions of cultural competence instruction in the
first three years of the curriculum.
Academic Medicine, 81,
557–564.
doi:10.1097/01.ACM.0000225219.53325.52
Lie, D. A., Boker, J., Crandall, S., DeGannes, C. N., Elliott, D., Henderson, P., … Seng, L. (2008). Revising
the tool for assessing cultural competence training (TACCT) for curriculum evaluation: Findings derived
from seven US schools and expert consensus.
Medical Education Online, 13
(11)
,
1
–
11.
doi:10.3885/meo.2008.Res00272
Lie, D. A., Lee-Rey, E., Gomez, A., Bereknyei, S., & Braddock, C. H., 3rd. (2010). Does cultural
competency training of health professionals improve patient outcomes? A systematic review and
proposed algorithm for future research.
Journal of General Internal Medicine, 26
(3), 317–325.
doi:10.1007/s11606-010-1529-0
Like, R. C. (2001).
Clinical cultural competency questionnaire.
Retrieved from Robert Wood Johnson
Medical School website:
http://rwjms.umdnj.edu/departments_institutes/family_medicine/chfcd/grants_projects/aetna.html
Like, R. C. (2011). Educating clinicians about cultural competence and disparities in health and health
care.
Journal of Continuing Education in the Health Professions, 31
(3), 196–206.
Like, R. C., Steiner, R. P., & Rubel, A. J. (1996). Recommended core curriculum guidelines on culturally
sensitive and competent health care.
Family Medicine, 28,
291–297. Retrieved from
http://www.stfm.org/corep.html
Liteman, M., Campbell, S., & Liteman, J. (2006).
Retreats that work:
Everything you need to know about
planning and leading great offsites.
San Francisco, CA: Pfeiffer.
Management Sciences for Health. (n.d.).
The provider’s guide to quality & culture.
Retrieved from
http://erc.msh.org/mainpage.cfm?file=1.0.htm&module=provider&language=English
McDougle, L., Ukockis, G., & Adamshick, L. (2010). Evaluation of a new cultural competency training
program: CARE Columbus.
Journal of the National Medical Association, 102
(9), 756–760.
National Council on Interpreting in Health Care. (2004).
A national code of ethics for interpreters in
health care.
Retrieved from http://www.oregon.gov/OHA/oei/intrprtr/docs/NCIHC_NCE.pdf
National Hispanic Health Foundation & the Josiah Macy, Jr. Foundation. (2009).
Increasing diversity in
the health professions: Recommendations to improve Title VII of the Public Health Service Act
. Retrieved
from http://josiahmacyfoundation.org/docs/grantee_pubs/NHHF-Macy_PHSA_Recs.pdf
National Quality Forum. (2009).
Safe practices for better healthcare–2009 update: A consensus report.
Retrieved from
http://www.qualityforum.org/Publications/2009/03/Safe_Practices_for_Better_Healthcare%e2%80%932
009_Update.aspx
Paez, K. A., Allen, J. K., Carson, K. A., & Cooper, L. A. (2008). Provider and clinic cultural competence in
a primary care setting.
Social Science and Medicine, 66
(5), 1204–1216. Retrieved from
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2426909/?tool=pubmed
Patient-Centered Primary Care Collaborative.
(n.d.). Retrieved from http://www.pcpcc.net
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 180
Theme 1 Resources
Powell, L., & Taylor, C. (2004).
Hospital governing board assessment: A self-help guide.
Boise, ID:
Mountain States Group.
Price, E. G., Beach, M. C., Gary, T. L., Robinson, K. A., Gozu, A., Palacio, A., ... Cooper, L. A. (2005). A
systematic review of the methodologic rigor of studies evaluating cultural competence training of health
professionals.
Academic Medicine, 80,
578–586. Retrieved from
http://journals.lww.com/academicmedicine/Fulltext/2005/06000/A_Systematic_Review_of_the_Methodol
ogical_Rigor_of.13.aspx
Quality interactions: A patient-based approach to cross-cultural care.
(2011). Retrieved from
http://www.qualityinteractions.org
Ring, J., Nyquist, J., Mitchell, S., Flores, H., & Samaniego, L. (2008).
Curriculum for culturally responsive
health care: The step-by-step guide for cultural competence training.
Oxford, UK: Radcliffe Publishing.
Schyve, P. M., & The Governance Institute. (2009).
Leadership in healthcare organizations: A guide to
Joint Commission leadership standards
. Retrieved from
http://www.jointcommission.org/assets/1/18/WP_Leadership_Standards.pdf
Sequist, T. D., Fitzmaurice, G. M., Marshall, R., Shaykevich, S., Marston, A., Safran, D. G., & Ayanian, J.
Z. (2010). Cultural competency training and performance reports to improve diabetes care for black
patients: A cluster randomized, controlled trial.
Annals of Internal Medicine, 152
(1), 40–46.
Smedley, B. D., Stith-Butler, A., & Bristow, L. R. (2004).
In the nation’s compelling interest: Ensuring
diversity in the health-care workforce.
Retrieved from
http://www.nap.edu/openbook.php?record_id=10885&page=1
The Sullivan Commission on Diversity in the Healthcare Workforce. (2004).
Missing persons: Minorities in
the health professions.
Retrieved from http://www.aacn.nche.edu/media-relations/SullivanReport.pdf
U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. (n.d.).
Training and continuing education online:
Health literacy for public health professionals (web-based)
[Online training course summary]. Retrieved from
http://www2a.cdc.gov/tceonline/registration/detailpage.asp?res_id=2074
U.S. Department of Health and Human Services, Health Resources and Services Administration. (n.d.).
Unified health communication 101.
Retrieved from
http://www.hrsa.gov/publichealth/healthliteracy/index.html
U.S. Department of Health and Human Services, Office of Minority Health. (2005).
A patient-centered
guide to implementing language access services in healthcare organizations.
Retrieved from
http://minorityhealth.hhs.gov/Assets/pdf/Checked/HC-LSIG.pdf
U.S. Department of Health and Human Services, Office of Minority Health. (n.d.).
A physician’s practical
guide to culturally competent care.
Retrieved from https://cccm.thinkculturalhealth.hhs.gov/
U.S. Department of Health and Human Services, Office of Minority Health. (n.d.).
Cultural competency
curriculum for disaster preparedness and crisis response.
Retrieved from
https://cccdpcr.thinkculturalhealth.hhs.gov/
U.S. Department of Health and Human Services, Office of Minority Health. (n.d.).
Culturally competent
nursing care: A cornerstone of caring.
Retrieved from https://ccnm.thinkculturalhealth.hhs.gov/
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 181
Theme 1 Resources
Virtual Lecture Hall. (2012).
Communicating through health care interpreters
[Online training course
summary]. Retrieved from http://www.vlh.com/shared/courses/course_info.cfm?courseno=155
Wynia, M. K., Johnson, M., McCoy, T. P., Passmore Griffin, L., & Osborn, C. Y. (2010). Validation of an
organizational communication climate assessment toolkit.
American Journal of Medical Quality, 25
(6),
436–443. doi:10.1177/1062860610368428
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 182
Theme 2 Resources
Adelson, B. L., & Bromberg & Associates, LLC. (2010).
Title VI for healthcare and healthcare-related
organizations
[Online training module]. Hamtramck, MI: Bromberg Translation Services.
American Medical Association Foundation. (2007).
Health literacy and patient safety: Help your patients
understand
[Educational kit]. Chicago, IL: American Medical Association Foundation.
American Medical Association. (n.d.).
C-CAT: Patient centered communication.
Retrieved from
http://www.ama-assn.org/go/ccat
American Medical Association. (2007).
Office guide to communicating with limited English proficient
patients
. Retrieved from http://www.ama-assn.org/ama1/pub/upload/mm/433/lep_booklet.pdf
American Speech-Language-Hearing Association. (2012).
National Joint Committee for the
Communication Needs of Persons with Severe Disabilities (NJC)
. Retrieved from http://www.asha.org/njc
Anderson, C. C., & National Council on Interpreting in Health Care (2002).
Linguistically appropriate
access and services: An evaluation and review for healthcare organizations.
Retrieved from
http://data.memberclicks.com/site/ncihc/NCIHC%20Working%20Paper%20-
%20Linguistically%20Appropriate%20Access%20and%20Services.pdf
Andrulis, D. P., & Brach, C. (2007). Integrating literacy, culture, and language to improve health care
quality for diverse populations.
American Journal of Health Behavior, 31,
S122–S133. Retrieved from
http://www.cpehn.org/pdfs/Integrating%20Literace%20Paper%20-%20Andrulis.pdf
Andrus, M. R., & Roth, M. T. (2002). Health literacy: A review.
Pharmacotherapy, 22
(3), 282–302.
Retrieved from www.cce.uri.edu/pharmacy/rotationdescriptions/Andrus_Wk2.pdf
Berger, C. (2005).
Universal symbols in health care workbook.
Retrieved from Hablamos Juntos website:
http://www.hablamosjuntos.org/signage/PDF/Best%20Practices-FINALDec05.pdf
Berkman, N. D., Sheridan, S. L., Donahue, K. E., Halpern, D. J., & Crotty, K. (2011). Low health literacy
and health outcomes: An updated systematic review.
Annals of Internal Medicine, 155
(2), 97–107.
Brach C., Keller, D, Hernandez, L., Baur, C., Parker, R., Schyve, P., Lemerise, & Schillinger, D. (2012).
Ten Attributes of Health Literate Health Care Organizations. Washington DC. Retrieved from:
http://www.iom.edu/Activities/PublicHealth/HealthLiteracy.aspx
Brach, C., Fraser, I., & Perez, K. (2005). Crossing the language chasm.
Health Affairs, 24
(2), 424–434.
doi:10.1377/hlthaff.24.2.424
California Academy of Family Physicians. (2005).
Addressing language access issues in your practice: A
toolkit for physicians and their staff members.
Retrieved from
http://www.calendow.org/uploadedFiles/language_access_issues.pdf
California Healthcare Interpreting Association.
(n.d.). Retrieved from http://chiaonline.org/
Centers for Medicare & Medicaid Services. (2011).
The toolkit for making written material clear and
effective: Overview.
Retrieved from https://www.cms.gov/WrittenMaterialsToolkit/
Certification Commission for Healthcare Interpreters.
(n.d.). Retrieved from
http://www.healthcareinterpretercertification.org/
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 183
Theme 2 Resources
Chen, A. (2006). Doctoring across the language divide.
Health Affairs, 25
(3), 808–813.
doi:10.1377/hlthaff.25.3.808
Chen, A. H., Youdelman, M. K., & Brooks, J. (2007). The legal framework for language access in
healthcare settings: Title VI and beyond.
Journal of General Internal Medicine, 22
(Supplement 2), 362–
367. doi:10.1007/s11606-007-0366-2
Commonwealth of Massachusetts Executive Office of Health and Human Services, Massachusetts
Department of Public Health. (2004).
Best practice recommendations for hospital-based interpreter
services.
Retrieved from
http://www.hablamosjuntos.org/pdf_files/Best_Practice_Recommendations_Feb2004.pdf
Cross-Cultural Communication Systems, Inc.
(2010). Retrieved from http://www.embracingculture.com
The Cross Cultural Health Care Program. (n.d.).
Communicating effectively through an interpreter
[DVD].
Seattle, WA: The Cross Cultural Health Care Program.
Divi, C., Koss, R. G., Schmaltz, S. P., & Loeb, J. M. (2007). Language proficiency and adverse events in
US hospitals: A pilot study.
International Journal of Quality in Health Care, 19
(2), 60–67.
doi:10.1093/intqhc/mzl069
Downing, B., & Bogoslaw, L. (2003).
Translation as a strategy for effective communication with patients
and clients: A how-to guide.
Retrieved from Hablamos Juntos website:
http://www.hablamosjuntos.org/pdf_files/BruceDowningHow-To_Guide_FINAL.pdf
Ferguson, L. A., & Pawlak, R. (2011). Health literacy: The road to improved health outcomes.
Journal for
Nurse Practitioners, 7
(2), 123–129. doi:10.1016/j.nurpra.2010.11.020
Gilbert, M. J., Partida, Y., Goode, T., & Dunne, C. (2005). Process of inquiry: Communicating in a
multicultural environment. In
Curricula enhancement module series.
Retrieved from the National Center
for Cultural Competence website: http://www.nccccurricula.info/communication/index.html
Grubbs, V., Chen, A. H., Bindman, A. B., Vittinghoff, E., & Fernandez, A. (2006). Effect of awareness of
language law on language access in the health care setting.
Journal of General Internal Medicine, 21
(7),
683–688. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1924696/?tool=pubmed
Hablamos Juntos: Language policy and practice in health care.
(n.d.). Retrieved from
http://www.hablamosjuntos.org
Hablamos Juntos. (2008).
Language testing options 2008.
Retrieved from
http://www.imiaweb.org/uploads/pages/218.pdf
Harvard School of Public Health. (2010).
Health literacy studies: Assessing and developing health
materials.
Retrieved from http://www.hsph.harvard.edu/healthliteracy/practice/innovative-
actions/index.html
Health Care Interpreter Network, Kaiser Permanente, & Casa Madre Films. (2009).
Qualified interpreting
for quality health care
[DVD]. Retrieved from http://vimeo.com/7225401
Health Literacy Innovations. (2008).
The health literacy & plain language resource guide.
Retrieved from
http://www.healthliteracyinnovations.com/information/RGdownload

National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 184
Theme 2 Resources
Hunt, D., & Walker, P. F. (2010).
Language access and the law: Caring for the LEP patient
[E-learning
program]. Minneapolis, MN: Critical Measures.
International Medical Interpreters Association. (1995).
Medical interpreting standards of practice.
Retrieved from http://www.hablamosjuntos.org/resources/pdf/IMIA_Standards_Of_Practice.pdf
International Medical Interpreters Association.
(2012). Retrieved from
http://www.imiaweb.org/default.asp
The Joint Commission. (2010).
Advancing effective communication, cultural competence, and patient-
and family-centered care: A roadmap for hospitals.
Retrieved from
http://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf
Kelly, N. (2007).
Telephone interpreting in health care settings: Some commonly asked questions
.
Retrieved from The ATA Chronicle website:
http://www.atanet.org/chronicle/feature_article_june2007.php
Kelly, N. (2008).
A medical interpreter’s guide to telephone interpreting
. Retrieved from International
Medical Interpreters Association website: http://www.imiaweb.org/uploads/pages/380.pdf
Kuo, D. Z., O'Connor, K. G., Flores, G., & Minkovitz, C. S. (2007). Pediatricians’ use of language services
for families with limited English proficiency.
Pediatrics 119
(4), e920–e27. doi:10.1542/peds.2006-1508.
Limited English proficiency: A federal interagency website.
(n.d.). Retrieved from http://www.lep.gov
LinguaLinks Library. (1999).
Correspondence of proficiency scales
. Retrieved from
http://www.sil.org/lingualinks/LANGUAGELEARNING/MangngYrLnggLrnngPrgrm/CorrespondenceOfProfici
encySca.htm
Meyers, K., Tang, G., & Fernandez, A. (2009). Responding to the language challenge: Kaiser
Permanente’s approach.
The Permanente Journal, 13
(3), 77–83. Retrieved from
http://www.thepermanentejournal.org/files/Summer2009/language_challenge.pdf
National Association of the Deaf.
(2012). Retrieved from http://www.nad.org/
National Board of Certification for Medical Interpreters.
(2012). Retrieved from
http://www.certifiedmedicalinterpreters.org/
National Council on Interpreting in Health Care.
(2011). Retrieved from http://www.ncihc.org
National Council on Interpreting in Health Care. (2001).
Guide to initial assessment of interpreter
qualifications.
Retrieved from
http://data.memberclicks.com/site/ncihc/NCIHC%20Working%20Paper%20Guide%20to%20Initial%20As
sessment%20of%20Interpreter%20Qualifications.pdf
National Council on Interpreting in Health Care. (2003).
Guide to interpreter positioning in health care
settings.
Retrieved from http://data.memberclicks.com/site/ncihc/NCIHC%20Working%20Paper%20-
%20Guide%20to%20Interpreter%20Positioning%20in%20Health%20Care%20Settings.pdf
National Council on Interpreting in Health Care. (2005).
National standards of practice for interpreters in
health care.
Retrieved from
http://mchb.hrsa.gov/training/documents/pdf_library/National_Standards_of_Practice_for_Interpreters_i
n_Health_Care%20(12-05).pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 185
Theme 2 Resources
National Council on Interpreting in Health Care. (2010).
Sight translation and written translation:
Guidelines for healthcare interpreters.
Retrieved from
http://data.memberclicks.com/site/ncihc/Translation%20Guidelines%20for%20Interpreters%20REVISED
%2031710.pdf
National Health Law Program. (2010).
What's in a word? A guide to understanding interpreting and
translation in health care.
Retrieved from
http://www.healthlaw.org/images/stories/Whats_in_a_Word_Guide.pdf
National Health Law Program. (2010).
Language access.
Retrieved from
http://www.healthlaw.org/index.php?option=com_content&id=239&Itemid=196
Osborne, H. (2001, November).
In other words…Can they understand? Testing patient education
materials with intended readers.
Retrieved from http://www.healthliteracy.com/article.asp?PageID=3811
(Reprinted from the
Boston Globe On Call
magazine)
Paras, M. (2005).
Straight talk: Model hospital policies and procedures on language access.
Retrieved
from http://www.calendow.org/uploadedFiles/straight_talk_model_hospital_policies.pdf
Pierce, L. (2010). How to choose and develop written educational materials.
Rehabilitation Nursing,
35
(3), 99–105. Retrieved from http://www.rehabnurse.org/pdf/rnj320.pdf
Plain Language Association International.
(2011). Retrieved from http://www.plainlanguagenetwork.org/
Quan, K., & Lynch, J. (2010).
The high costs of language barriers in medical malpractice.
Retrieved from
National Health Law Program website:
http://www.healthlaw.org/images/stories/High_Costs_of_Language_Barriers_in_Malpractice.pdf
Registry of Interpreters for the Deaf. (2012).
Standard practice papers.
Retrieved from
http://www.rid.org/interpreting/Standard%20Practice%20Papers/index.cfm
Registry of Interpreters for the Deaf.
(2012). Retrieved from http://www.rid.org
Roat, C. E. (2005).
Assessing language access issues in your practice: A toolkit for physicians and their
staff members.
Retrieved from The California Endowment website:
http://www.calendow.org//uploadedFiles//language_access_issues.pdf
Robert Wood Johnson Foundation. (2008).
Kaiser Permanente’s health care interpreter certificate
program.
Retrieved from http://www.rwjf.org/pr/product.jsp?id=34036
Robert Wood Johnson Foundation. (2008).
Kaiser Permanente’s qualified bilingual staff model.
Retrieved
from http://www.rwjf.org/pr/product.jsp?id=34030
Robert Wood Johnson Foundation. (2008).
Speaking together toolkit.
Retrieved from
http://www.rwjf.org/pr/product.jsp?id=29653
Robert Wood Johnson Foundation. (n.d.).
Shared decision-
making when an interpreter is needed: A case
study with Latino men at risk for prostate cancer
(Grant details). Retrieved from
http://www.rwjf.org/grants/grant.jsp?id=63830
Tang, G., Lanza, O., & Rodriguez, F. M. (2011). Case study: The language of diversity.
Diversity
Executive,
44–46. Retrieved from http://diversity-executive.com/articles/view/1160
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 186
Theme 2 Resources
Tang, G., Lanza, O., Rodriguez, F. M., & Chang, A. (2011). The Kaiser clinician cultural and linguistic
assessment initiative: Research and development in patient-provider language concordance.
American
Journal of Public Health, 101
(2), 205–208.
Trott, J., West, C., Shah, P., & Regenstein, M. (2008).
Building a high-quality language services program
toolkit.
Retrieved from http://www.lawhelp.org/documents/391611Building%20a%20High-
Quality%20Language%20Services%20Program%20Toolkit.pdf
Txabarriaga, R. (2009).
IMIA guide on medical translation.
Retrieved from International Medical
Interpreters Association website: http://www.imiaweb.org/uploads/pages/438.pdf
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2011).
CAHPS item set for addressing health literacy
. Retrieved from https://www.cahps.ahrq.gov/surveys-
guidance/item-sets/health-literacy.aspx
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2010).
Health literacy universal precautions toolkit
(AHRQ Publication No. 10-0046-EF). Retrieved from
http://www.ahrq.gov/qual/literacy/
U.S. Department of Health and Human Services, Office for Civil Rights. (2003).
Guidance to federal
financial assistance recipients regarding Title VI and the prohibition against national origin discrimination
affecting limited English proficient persons.
Retrieved from
http://www.hhs.gov/ocr/civilrights/resources/laws/revisedlep.html
U.S. Department of Justice, Civil Rights Division. (n.d.).
Federal agency LEP guidance & language access
plans.
Retrieved from http://www.lep.gov/guidance/guidance_index.html
U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion.
(2010).
Health literacy online: A guide to writing and designing easy-to-use health web sites.
Retrieved
from http://www.health.gov/healthliteracyonline
U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion.
(2010).
National action plan to improve health literacy.
Retrieved from
http://www.health.gov/communication/HLActionPlan/pdf/Health_Literacy_Action_Plan.pdf
U.S. Department of Health and Human Services, Office of Minority Health. (2005).
A patient-centered
guide to implementing language access services in healthcare organizations.
Retrieved from
http://minorityhealth.hhs.gov/Assets/pdf/Checked/HC-LSIG.pdf
Virtual Lecture Hall. (2012).
Communicating through health care interpreters
[Online training course
summary]. Retrieved from http://www.vlh.com/shared/courses/course_info.cfm?courseno=155
Wynia, M. K., Johnson, M., McCoy, T. P., Passmore Griffin, L., & Osborn, C. Y. (2010). Validation of an
organizational communication climate assessment toolkit.
American Journal of Medical Quality, 25
(6),
436–443. doi:10.1177/1062860610368428
Wynia, M., & Matiasek, J. (2006).
Promising practices for patient-centered communication with
vulnerable populations: Examples from eight hospitals
(Commonwealth Fund Publication No. 947).
Retrieved from The Commonwealth Fund website:
http://www.commonwealthfund.org/~/media/Files/Publications/Fund%20Report/2006/Aug/Promising%2
0Practices%20for%20Patient%20Centered%20Communication%20with%20Vulnerable%20Populations%
20%20Examples%20from%20Ei/Wynia_promisingpracticespatientcentered_947%20pdf.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 187
Theme 3 Resources
American Medical Association. (n.d.).
C-CAT: Patient centered communication.
Retrieved from
http://www.ama-assn.org/go/ccat
Asset-Based Community Development Institute.
(2009). Retrieved from http://www.abcdinstitute.org/
Association of the Bar of the City of New York. (n.d.).
Diversity committees that make a difference.
Retrieved from
http://www.akcsystems.com/test3/images/stories/pdfs/Diversity%20Committee%20Notes%20Article10_
2004.pdf
Aubel, J. (1999).
Participatory program evaluation manual: Involving program stakeholders in the
evaluation process.
Retrieved from http://www.idrc.ca/uploads/user-
S/10504133390Participatory_Program_Evaluation_Manual.pdf
Baker, Q. E., Davis, D. A., Gallerani, R., Sanchez, V., Viadro, C., & The Center for the Advancement of
Community Based Public Health. (2000).
An evaluation framework for community health programs.
Retrieved from http://www.doh.state.fl.us/COMPASS/documents/Community_Health_Programs_Eval.pdf
Baker, S., Conrad, D., Béchamps, M., & Barry M. (2002).
Healthy people toolkit 2010: A field guide to
health planning.
Retrieved from Public Health Foundation website:
http://www.phf.org/resourcestools/Documents/HP2010Toolkit2002.pdf
Beach, M. C., Cooper, L. A., Robinson, K. A., Price, E. G., Gary, T. L., Jenckes, M. W., … Powe, N. R.
(2004).
Strategies for improving minority healthcare quality
(AHRQ Publication No. 04-E008-02).
Retrieved from Agency for Healthcare Research and Quality website:
http://archive.ahrq.gov/downloads/pub/evidence/pdf/minqual/minqual.pdf
Betancourt, J. R., Weissman, J. S., Kim, M. K., Park, E., & Maina, A. W. (2007).
Resident physicians’
preparedness to provide cross-cultural care: Implications for clinical care and medical education policy
.
Retrieved from The Commonwealth Fund website:
http://www.commonwealthfund.org/usr_doc/1026_Betancourt_resident_MDs_preparedness_provide_cro
ss-cultural_care.pdf
Bhui, K., Warfa, N., Edonya, P., McKenzie, K., & Bhugra, D. (2007). Cultural competence in mental health
care: A review of model evaluations.
BMC Health Services Research, 7,
15. doi:10.1186/1472-6963-7-15
Campinha-Bacote, J. (2002).
Inventory for assessing the process of cultural competence among
healthcare professionals-revised (IAPCC-R).
Retrieved from http://www.transculturalcare.net/iapcc-r.htm
CASAS.
(2011). Retrieved from https://www.casas.org
Johns Hopkins University. (2010).
COA360.
Retrieved from http://www.COA360.org
Clinical and Translational Science Awards Consortium, Community Engagement Key Function Committee
Task Force on the Principles of Community Engagement. (2011).
Principles of community engagement
(2nd ed.) (National Institutes of Health Publication No. 11-7782). Retrieved from
http://www.atsdr.cdc.gov/communityengagement/pdf/PCE_Report_508_FINAL.pdf
Cummings, L. C., Bennett, B. A., Boutwell, A. E., & Martinez, E. L. (2008).
Assuring healthcare quality: A
healthcare equity blueprint.
Retrieved from
http://www2.massgeneral.org/disparitiessolutions/resources.html
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 188
Theme 3 Resources
Dator, J. (1991).
Culturally-appropriate dispute resolution techniques and the formal judicial system in
Hawaii. A report to the state justice institute.
Retrieved from
http://www.futures.hawaii.edu/publications/courts/CultAppropAD1991.pdf
Drucker, P. F. (1998).
The Drucker Foundation self-assessment tool: Participant workbook.
Hoboken, NJ:
Jossey-Bass, Inc.
DuPraw, M., & Axner, M. (2011).
Working on common cross-cultural communication challenges.
Retrieved from http://www.pbs.org/ampu/crosscult.html
Fiscella, K. (2011). Eliminating disparities in health care through quality improvement. In R. A. Williams
(Ed.),
Healthcare disparities at the crossroads with healthcare reform
(pp. 231–267). New York, NY:
Springer.
Hasnain-Wynia, R., & Baker, D. W. (2006). Obtaining data on patient race, ethnicity, and primary
language in health care organizations: Current challenges and proposed solutions.
Health Services
Research, 41,
1501–1518. doi:10.1111/j.1475-6773.2006.00552.x
Hasnain-Wynia, R., Pierce, D., Haque, A., Hedges Greising, C., Prince, V., & Reiter, J. (2007).
Health
Research and Educational Trust disparities toolkit.
Retrieved from http://www.hretdisparities.org/
Hasnain-Wynia, R., Van Dyke, K., Youdelman, M., Krautkramer, C., Ivey, S., Gilchick, R., Kaleba, E., &
Wynia M. (2010). Barriers to collecting patient race, ethnicity and primary language data in physician
practices: An exploratory study.
Journal of the National Medical Association, 102
(9), 769–775.
Institute for Patient- and Family-Centered Care. (2011).
Tools to foster the collaboration with patient and
family advisors.
Retrieved from http://www.ipfcc.org/tools/downloads-tools.html
Johnson, M. J., & Kanitsaki, O. (2006). Culture, language, and patient safety: Making the link.
International Journal of Quality in Health Care, 18,
383–388. Retrieved from
http://intqhc.oxfordjournals.org/content/18/5/383.full.pdf
The Joint Commission. (2007).
“What did the doctor say?”: Improving health literacy to protect patient
safety.
Retrieved from http://www.jointcommission.org/assets/1/18/improving_health_literacy.pdf
Lahey Clinic Foundation.
(2012). Retrieved from http://www.lahey.org/
LeBaron, M. (1998).
Mediation and multicultural reality.
Retrieved from
http://www.gmu.edu/programs/icar/pcs/lebaron.htm
Leonhardt, K., Bonin, D., & Pagel, P. (2008).
Guide for developing a community-based patient safety
advisory council
(AHRQ Publication No. 08-0048). Retrieved from
http://www.ahrq.gov/qual/advisorycouncil/advisorycouncil.pdf
Management Sciences for Health. (n.d.).
The provider’s guide to quality & culture.
Retrieved from
http://erc.msh.org/mainpage.cfm?file=1.0.htm&module=provider&language=English
Mind Tools. (n.d.).
Conflict resolution: Resolving conflict rationally and effectively.
Retrieved from
http://www.mindtools.com/pages/article/newLDR_81.htm
National Center for Cultural Competence, Georgetown University Center for Child and Human
Development, Georgetown University Medical Center. (2004).
Bridging the cultural divide in health care
setting: The essential role of cultural broker programs.
Retrieved from
http://gucchd.georgetown.edu/products/CulturalBrokerGuide_English.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 189
Theme 3 Resources
National Center for Cultural Competence, Georgetown University Center for Child and Human
Development, Georgetown University Medical Center. (n.d.).
Cultural competence health practitioner
assessment (CCHPA).
Retrieved from http://nccc.georgetown.edu/features/CCHPA.html
National Committee for Quality Assurance. (2011).
Recognizing innovations in multicultural health care.
Retrieved from http://www.ncqa.org/tabid/453/Default.aspx
National Consensus Panel on Emergency Preparedness and Cultural Diversity. (2011).
Guidance for
integrating culturally diverse communities into planning for and responding to emergencies: A toolkit
(HHS Office of Minority Health Publication No. OMH-NHMA-5-10). Retrieved from
http://www.hhs.gov/ocr/civilrights/resources/specialtopics/emergencypre/omh_diversitytoolkit.pdf
National Quality Forum. (2008).
National voluntary consensus standards for ambulatory care: Measuring
healthcare disparities.
Retrieved from
http://www.qualityforum.org/Publications/2008/03/National_Voluntary_Consensus_Standards_for_Ambul
atory_Care%E2%80%94Measuring_Healthcare_Disparities.aspx
National Quality Forum. (n.d.).
Cultural competency 2010: Cultural competency measures and
implementation strategies.
Retrieved from http://www.qualityforum.org/Projects/c-
d/Cultural_Competency_2010/Cultural_Competency_2010.aspx
Ohmans, P., & Cushing, M. (2000).
Getting the word out: Effective health outreach to cultural
communities.
Retrieved from The Medtronic Foundation website:
http://www.medtronic.com/downloadablefiles/outreach_brochure.pdf
Rice, M. F. (2007). Promoting cultural competency in public administration and public service delivery:
Utilizing self-assessment tools and performance measures.
Journal of Public Affairs Education, 13,
41–57.
Roat, C. (2003).
How to choose and use a language agency: A guide for health and social service
providers who wish to contract with language agencies.
Retrieved from The California Endowment
website: http://www.calendow.org/uploadedFiles/how_to_choose_use_language_agency.pdf
Rogers, S., & Vilhena, B. (2005). Benchmarking patient complaints data across Ontario hospitals:
University Health Network invites collaboration [Online case study].
Healthcare Quarterly.
Retrieved from
http://www.longwoods.com/product/download/code/17728
San Francisco Department of Public Health.
(n.d.). Retrieved from http://www.sfdph.org/dph/default.asp
Sandrick, K. (2006). Defining and measuring community benefit.
Trustee, 59
(9), 6–10. Retrieved from
http://www.trusteemag.com/trusteemag_app/jsp/articledisplay.jsp?dcrpath=TRUSTEEMAG/PubsNewsArt
icleGen/data/2006October/0610TRU_CoverStory&domain=TRUSTEEMAG
Schillinger, D. (2010).
An introduction to effectiveness, dissemination and implementation research: A
resource manual for community-engaged research.
Retrieved from
http://accelerate.ucsf.edu/files/CE/edi_introguide.pdf
Sharpe, P. A., Greaney, M. L., Lee, P. R., & Royce, S. W. (2000). Assets-oriented community assessment.
Public Health Reports, 115,
205–211. Retrieved from
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1308712/pdf/pubhealthrep00022-0103.pdf
Snowden, L. R. (2003).
Toward culturally competent evaluation in health and mental health.
Retrieved
from The California Endowment website:
http://www.calendow.org/uploadedFiles/Publications/Evaluation/toward_culturally_competent_evaluation
.pdf
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 190
Theme 3 Resources
Summit Health Institute for Research and Education. (2004).
Building coalitions among communities of
color: A multicultural approach.
Retrieved from http://www.shireinc.org/wp-
content/files/Building_Coalitions_among_Communities_of_Color.pdf
Thom, D. H., & Tirado, M. D. (2006). Development and validation of a patient-reported measure of
physician cultural competency.
Medical Care Research and Review, 63
(5), 636–655.
doi:10.1177/1077558706290946
Torres, G., & Margolin, F. (2003).
The collaboration primer: Proven strategies, considerations, and tools
to get you started.
Retrieved from Health Research and Educational Trust website:
http://www.hret.org/upload/resources/collaboration-primer.pdf
Townsend, J. R. (2011). Creating a culturally and politically appropriate dispute resolution model:
Working in Indian country.
RCAC's Rural Review, 28
(3), 1–7. Retrieved from
http://www.rcac.org/assets/white-papers/CreatingACulturally.pdf
University of Colorado Conflict Information Consortium
. (n.d.). Retrieved from
http://conflict.colorado.edu/
University of Washington, Community-Campus Partnerships for Health. (n.d.).
Community-based
participatory research.
Retrieved from http://depts.washington.edu/ccph/commbas.html
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2008).
Hospital language services: Quality improvement and performance measures. In
Advances in patient
safety: New directions and alternative approaches, Volume 2. Culture and redesign.
(AHRQ Publication
No. 08-0034-2). Retrieved from http://www.ncbi.nih.gov/books/NBK43719
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2011).
CAHPS cultural competence item set.
Retrieved from https://www.cahps.ahrq.gov/surveys-
guidance/item-sets/cultural-competence.aspx
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2011).
CAHPS item set for addressing health literacy.
Retrieved from https://www.cahps.ahrq.gov/surveys-
guidance/item-sets/health-literacy.aspx
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2011).
CAHPS: Surveys and tools to advance patient-centered care.
Retrieved from http://www.cahps.ahrq.gov
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (n.d.).
National healthcare quality and disparities reports.
Retrieved from
http://www.ahrq.gov/qual/measurix.htm#quality
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. (2011).
Surveys on patient safety culture
. Retrieved from http://www.ahrq.gov/qual/patientsafetyculture/
U.S. Department of Health and Human Services, Health Resources and Services Administration. (2001).
Cultural competence works: Using cultural competence to improve the quality of health care for diverse
populations and add value to managed care arrangements.
Retrieved from
ftp://ftp.hrsa.gov/financeMC/cultural-competence.pdf
U.S. Department of Health and Human Services, Office of Minority Health. (2011).
Final data collection
standards for race, ethnicity, primary language, sex, and disability status required by Section 4302 of the
Affordable Care Act.
Retrieved from
http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlid=208
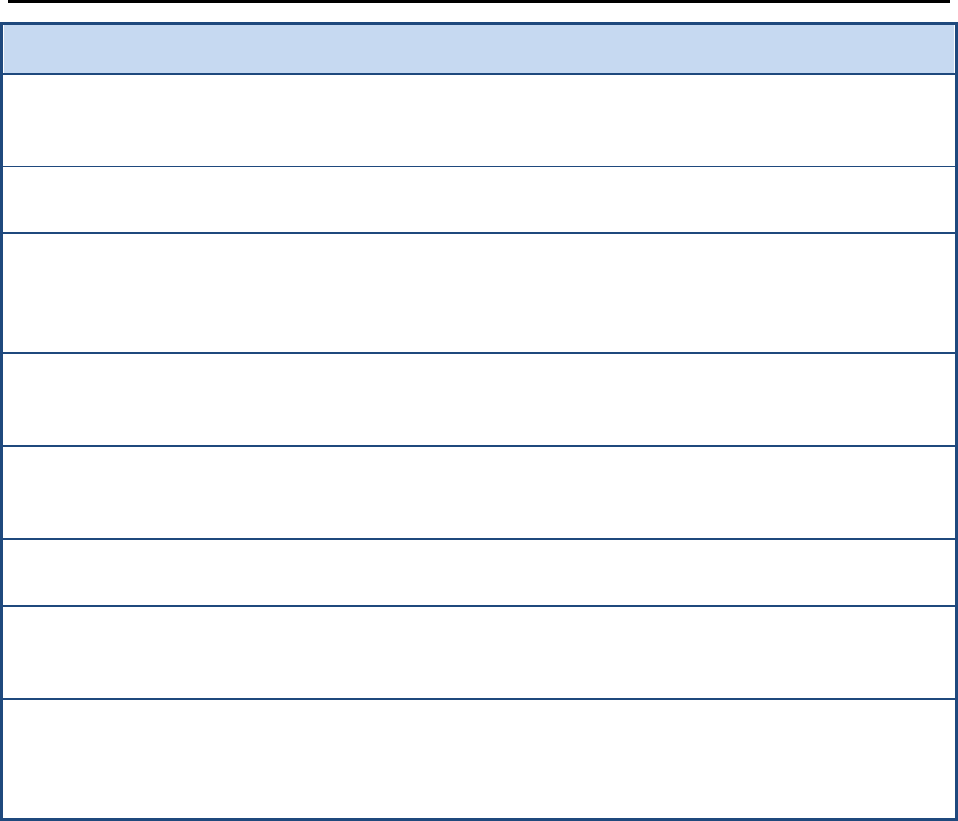
National Standards for CLAS in Health and Health Care:
A Blueprint for Advancing and Sustaining CLAS Policy and Practice
Appendix E: Resources 191
Theme 3 Resources
U.S. Department of Health and Human Services, Office of Minority Health. (2011).
Improving data for
the LGBT community.
Retrieved from
http://minorityhealth.hhs.gov/templates/content.aspx?lvl=2&lvlid=209&id=9004
U.S. Department of Commerce, Census Bureau. (n.d.).
American factfinder.
Retrieved from
http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml
Vogt, K. (2006, September). Mystery shopping gaining popularity in health care sector: The rise of
consumer-directed care is one reason why physicians, hospitals and health plans are sending people
incognito to learn how things are working.
American Medical News.
Retrieved from http://www.ama-
assn.org/amednews/2006/09/18/bise0918.htm
Wang, S. (2006, August 8). Health care taps “mystery shoppers”: To improve service, hospitals and
doctors hire spies to pose as patients and report back.
Wall Street Journal.
Retrieved from
http://online.wsj.com/article/SB115499684792929340.html
Weech-Maldonado, R. (2007, June).
Moving towards culturally competent health systems: Organizational
and market factors.
Presented at the AcademyHealth Disparities Interest Group Meeting, Orlando, FL.
Retrieved from http://www.academyhealth.org/files/interestgroups/disparities/weech-maldonador.pdf
Wilson-Stronks, A., & Galvez, E. (2007).
Hospitals, language, and culture: A snapshot of the nation.
Retrieved from The Joint Commission website: http://www.jointcommission.org/assets/1/6/hlc_paper.pdf
Wu, E., & Martinez, M. (2006).
Taking cultural competency from theory to action.
(Commonwealth Fund
Publication No. 964). Retrieved from The Commonwealth Fund website:
http://www.commonwealthfund.org/usr_doc/Wu_takingcultcomptheoryaction_964.pdf
Wynia, M., Hasnain-Wynia, R., Hotze, T. D., & Ivey, S. L. (2011).
Collecting and us
ing race, ethnicity and
language data in ambulatory settings: A white paper with recommendations from the Commission to End
Health Care Disparities.
Retrieved from American Medical Association website: http://www.ama-
assn.org/resources/doc/public-health/cehcd-redata.pdf
